Tirzepatide / Niacinamide Injection
This product is available through both our 503A Compounding Pharmacy and our 503B Outsourcing Facility, ensuring versatile solutions tailored to meet your needs. If you do not have an account, please contact us.
Product Overview
Tirzepatide
Tirzepatide functions as a dual GLP-1 and GIP agonist. Similar to other GLP-1 medicines, it is currently used as a second-line diabetic treatment and administered as a once-weekly subcutaneous injection.[1][2]
Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonist. It has not been tested on individuals with pancreatitis and is not approved to treat type-1 diabetes mellitus. As a GIP and GLP-1 receptor agonist, it is implemented as a second-line defense against type 2 diabetes for glycemic control and significantly reduces body weight.[1][3]
According to recent clinical studies, tirzepatide decreases hemoglobin A1C levels more effectively than a placebo. In comparison to -0.86% with placebo, the SURPASS-5 clinical trial revealed a -2.11% drop in hemoglobin A1C levels at 5mg per week dose. Hemoglobin A1C decreased by -2.34% when tirzepatide was taken at the maximum dose of 15 mg per week. This was proven during a 40-week period. With a tirzepatide dosage of 5 mg, a weight loss of 5.4 kg was observed, while a weight loss of 10.5 kg was observed with a dosage of 15 mg. A popular GLP-1 drug used for weight loss therapy is similar to this dose-dependent link with weight loss.[1][4]
Tirzepatide has been demonstrated to function similarly to GLP-1 medicines but more effectively. Given its ability to help people lose weight and absence of liver toxicity, it could help people with non-alcoholic fatty liver disease (NAFLD) in a secondary way.[1][5]
Niacinamide
Niacin, also known as nicotinic acid or vitamin B3, is a vital water-soluble B vitamin that may play a crucial role in various physiological functions. It may help support the metabolism of carbohydrates, fats, and proteins, facilitating the conversion of food into energy. Niacin may also help support healthy skin, nerves, and digestive systems.[11][12][13]
Dietary sources of niacin include a variety of foods such as animal proteins (e.g., poultry, beef, and fish), legumes, nuts, seeds, whole grains, and green vegetables. While niacin is present in cereal grains, it is often bound to polysaccharides, which may hinder absorption. To enhance dietary intake, refined grains are commonly enriched with niacin.[13][14] Additionally, the body can synthesize niacin from tryptophan, an amino acid found in protein. Approximately 60 mg of tryptophan can yield about 1 mg of niacin.[13]
Niacin serves as a precursor for the coenzymes NAD and NADP, which are critical for numerous biochemical reactions within the body. These coenzymes are involved in energy production and cellular function.[13] A niacin deficiency can lead to serious health issues, including pellagra. Pellagra is a condition characterized by dermatitis, diarrhea, and dementia. Niacin deficiency, although uncommon, may result from inadequate dietary intake or impaired tryptophan metabolism.[11][12][13][14]
Additionally, an animal study suggested niacinamide may influence whole-body energy expenditure by inducing phenotypic changes in adipose tissue in mice with diet-induced obesity. Further research is needed to determine niacinamide’s potential to aid in the prevention of obesity and its associated comorbidities.[15]
Tirzepatide is a synthetic peptide that acts as an agonist for both the glucagon-like peptide-1 (GLP-1) and gastric inhibitory polypeptide (GIP) receptors. It is a gastric inhibitory polypeptide mimic and has 39 amino acids. Functionally, it causes the pancreas to release more insulin, which lowers blood sugar levels. Adiponectin concentrations are similarly raised by tirzepatide. Its dual agonism ability decreases hunger and significantly lowers hyperglycemia compared to GLP-1 agonist drugs used alone.[1][6]
Tirzepatide causes thyroid C-cell tumors in rats. It is unknown whether Tirzepatide causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans as the human relevance of tirzepatide-induced rodent thyroid C-cell tumors has not been determined.
Tirzepatide is contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Counsel patients regarding the potential risk of MTC and symptoms of thyroid tumors.
Patients with Hepatic Impairment: No dosage adjustment of tirzepatide is suggested for patients with hepatic impairment.
Patients with Renal Impairment: Tirzepatide is associated with gastrointestinal ADRs, including nausea, vomiting, and diarrhea leading to dehydration, which can cause acute kidney injury. Use with caution in patients prone to dehydration.
In vitro studies have shown low potential for tirzepatide to inhibit or induce CYP enzymes, and to inhibit drug transporters. Tirzepatide delays gastric emptying, and thereby has the potential to impact the absorption of concomitantly administered oral medications.
The impact of tirzepatide on gastric emptying was greatest after a single dose of 5 mg and diminished after subsequent doses.
Following a first dose of tirzepatide 5 mg, acetaminophen maximum concentration (Cmax) was reduced by 50%, and the median peak plasma concentration (tmax) occurred 1 hour later. After coadministration at week 4, there was no meaningful impact on acetaminophen Cmax and tmax. Overall acetaminophen exposure (AUC0-24hr) was not influenced.
Following administration of a combined oral contraceptive (0.035 mg ethinyl estradiol and 0.25 mg norgestimate) in the presence of a single dose of tirzepatide 5 mg, mean Cmax of ethinyl estradiol, norgestimate, and norelgestromin was reduced by 59%,66%, and 55%, while mean AUC was reduced by 20%, 21%, and 23%, respectively. A delay in tmax of 2.5 to 4.5 hours was observed.
Based on available data, most users do not experience significant adverse drug reactions. The primary adverse effects reported are gastrointestinal, but other side effects have also been infrequently reported. Decreased appetite is frequently reported, though this is a potential contributory etiology of intentional weight loss. Below are the adverse drug reactions reported by System Organ Class (SOC).[1]
Gastrointestinal: Many people report having lowered appetite. Up to 10% of patients may experience nausea and diarrhea, and there may also be sporadic reports of vomiting and acid reflux. Additionally, some individuals have reported having constipation.[1][2] Other oral drugs have a harder time being absorbed when stomach emptying is delayed. This is especially important for people who already have delayed stomach emptying because it can make their symptoms worse. It is significant to highlight that oral hormonal contraceptives no longer work as well as they once did, so patients should be urged to use non-oral contraceptive methods instead. [1][2]
Cardiovascular: If discovered, sinus tachycardia may be suppressed by taking other medications concurrently.[2]
Renal: Acute renal injury has been documented in rare cases, most likely as a result of dehydration from gastrointestinal losses. These can happen to both healthy people and those who already have chronic renal illness. It is probably best to keep an eye out for indicators of dehydration to avoid kidney damage.
Dermatologic: Rarely, reports of hypersensitivity reactions at the injection site have been made. The prevalence is not more than what patients who use GLP-1 agonists report. Such occurrences should be handled with a doctor, who may also recommend stopping the prescription.
Pancreatitis: Acute pancreatitis is known to be a risk factor for GLP-1 drugs. Tirzepatide has a comparable level of risk as GLP-1 agonist drugs. If a patient receiving tirzepatide therapy experiences significant abdominal pain, they should be urged to visit their local emergency room for treatment. Some patients may also experience asymptomatic elevations of the enzymes lipase and amylase.[8]
Hepatobiliary: There have been reports of cholelithiasis and cholecystitis occurring in patients on tirzepatide therapy.[5]
Ocular: Patients with preexisting diabetic retinopathy should be advised that those symptoms may temporarily worsen if their glycemic control quickly improves. Any vision changes while using tirzepatide(GLP-1 receptor agonist) should be immediately discussed with a physician.[9]
Endocrine: There is a small risk of hypoglycemia and dose dependent. This risk is more significant for those on insulin therapy and/or those utilizing sulfonylureas. Patients should be advised on the potential symptoms of hypoglycemia.[10]
The amount of information on tirzepatide use during pregnancy is insufficient to evaluate the drug’s potential relation to congenital problems and poor maternal or fetal outcomes. An increased risk to the mother and fetus is linked to poorly managed pregnancy diabetes. Additionally, increased rates of skeletal, visceral, and exterior abnormalities have been noted in research on animal reproduction. Therefore, tirzepatide exposure during pregnancy can pose dangers to the fetus.[1]
As a result, tirzepatide should only be used during pregnancy if the benefit outweighs the danger to the fetus. Tirozepatide should only be provided to women of childbearing age after being fully evaluated for possible teratogenic effects. Before recommending tirzepatide, doctors should also talk about starting a contraceptive regimen. Additionally, while using tirzepatide medication, the effectiveness of oral hormonal contraception decreases.[1]
For at least four weeks following the start of tirzepatide therapy, barrier contraception should be used or switching to a non-oral method of contraception may need shared decision-making.[1]
There is no information on tirzepatide’s presence in human or animal milk or how it may affect a nursing infant. Therefore, physicians should take into account breastfeeding’s positive effects on growth and health, the mother’s clinical need for tirzepatide, and any potential side effects of tirzepatide on the breastfed child.
Tirzepatide is a large molecule with a high molecular weight. So the concentration of milk is accordingly less and probably destroyed in the infant’s digestive system and absorption is unlikely. Tirozepatide should therefore be used with caution during nursing, especially in newborn or preterm infants, until further clinical data are available.[1][7]
Upon receipt of medication, immediately store between 35°F to 46°F (2°C – 8°C). Keep all medicines out of the reach of children. Throw away any unused medicine within 28 days of puncture or the BUD, whichever comes first. Do not flush unused medications or pour them down a sink or drain.
- Farzam K, Patel P. Tirzepatide. [Updated 2023 May 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585056/
- Tirzepatide for type 2 diabetes.Med Lett Drugs Ther.2022 Jul 11;64(1654):105-107. https://pubmed.ncbi.nlm.nih.gov/35802842/
- Collins L, Costello RA. StatPearls [Internet].StatPearls Publishing; Treasure Island (FL): Jan 13, 2023. Glucagon-like Peptide-1 Receptor Agonists. https://pubmed.ncbi.nlm.nih.gov/31855395/
- Dahl D, Onishi Y, Norwood P, Huh R, Bray R, Patel H, Rodríguez Á. Effect of Subcutaneous Tirzepatide vs Placebo Added to Titrated Insulin Glargine on Glycemic Control in Patients With Type 2 Diabetes: The SURPASS-5 Randomized Clinical Trial. JAMA. 2022 Feb 08;327(6):534-545. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8826179/
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda (MD): Jun 20, 2022. Tirzepatide.
- Sun B, Willard FS, Feng D, Alsina-Fernandez J, Chen Q, Vieth M, Ho JD, Showalter AD, Stutsman C, Ding L, Suter TM, Dunbar JD, Carpenter JW, Mohammed FA, Aihara E, Brown RA, Bueno AB, Emmerson PJ, Moyers JS, Kobilka TS, Coghlan MP, Kobilka BK, Sloop KW. Structural determinants of dual incretin receptor agonism by tirzepatide. Proc Natl Acad Sci U S A. 2022 Mar 29;119(13):e2116506119. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9060465/
- Drugs and Lactation Database (LactMed®) [Internet]. National Institute of Child Health and Human Development; Bethesda (MD): Jun 20, 2022. Tirzepatide. https://pubmed.ncbi.nlm.nih.gov/35759552
- Trujillo J. Safety and tolerability of once-weekly GLP-1 receptor agonists in type 2 diabetes. J Clin Pharm Ther. 2020 Sep;45 Suppl 1(Suppl 1):43-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7540535/
- Bethel MA, Diaz R, Castellana N, Bhattacharya I, Gerstein HC, Lakshmanan MC. HbA1c Change and Diabetic Retinopathy During GLP-1 Receptor Agonist Cardiovascular Outcome Trials: A Meta-analysis and Meta-regression. Diabetes Care. 2021 Jan;44(1):290-296. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7783944/
- Chavda VP, Ajabiya J, Teli D, Bojarska J, Apostolopoulos V. Tirzepatide, a New Era of Dual-Targeted Treatment for Diabetes and Obesity: A Mini-Review. Molecules. 2022 Jul 05;27(13) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9268041/
- Niacin. (n.d.). Mayo Clinic. https://www.mayoclinic.org/drugs-supplements-niacin/art-20364984
- Niacin: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/002409.htm
- Office of Dietary Supplements – Niacin. (n.d.). https://ods.od.nih.gov/factsheets/Niacin-HealthProfessional/
- Office of Dietary Supplements – Niacin. (n.d.). https://ods.od.nih.gov/factsheets/Niacin-Consumer/
- Méndez‐Lara, K. A., Rodríguez‐Millán, E., Sebastián, D., Blanco‐Soto, R., Camacho, M., Nan, M. N., Diarte‐Añazco, E. M. G., Mato, E., Lope‐Piedrafita, S., Roglans, N., Laguna, J. C., Alonso, N., Mauricio, D., Zorzano, A., Villarroya, F., Villena, J. A., Blanco‐Vaca, F., & Julve, J. (2021). Nicotinamide protects against Diet‐Induced body weight gain, increases energy expenditure, and induces white adipose tissue beiging. Molecular Nutrition & Food Research, 65(11). https://doi.org/10.1002/mnfr.202100111
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
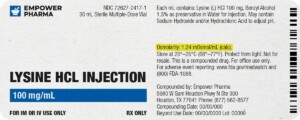
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.




 Sermorelin Acetate Injection
Sermorelin Acetate Injection Semaglutide / Cyanocobalamin Injection
Semaglutide / Cyanocobalamin Injection Testosterone Cypionate / Testosterone Propionate Injection
Testosterone Cypionate / Testosterone Propionate Injection Omnitrope Injection
Omnitrope Injection Ondansetron Tablets
Ondansetron Tablets Tirzepatide ODT
Tirzepatide ODT Sermorelin Acetate ODT
Sermorelin Acetate ODT Norditropin Injection
Norditropin Injection Testosterone Enanthate Injection
Testosterone Enanthate Injection Zomacton Injection
Zomacton Injection