Testosterone Cream
This product is available solely through our 503A Compounding Pharmacy, ensuring personalized care and precision in every order. Please note that a valid prescription is required for purchase. If you do not have an account, please contact us.
Product Overview
“The main androgen in the body is testosterone. Species of cells in the testis, ovary, and adrenal cortex produce endogenous testosterone. In the treatment of either congenital or acquired hypogonadism, testosterone is employed. The best exogenous androgen for the palliative therapy of breast cancer in postmenopausal women is testosterone. In 1938, testosterone was in use, and the FDA gave its approval in 1939. Since they have been used illegally, anabolic steroids, which are testosterone derivatives, are now considered controlled substances. In 1991, testosterone, along with a number of anabolic steroids, was designated as a restricted substance. AndroGel, a testosterone cream developed by Uniumed Pharmaceuticals in the US, received FDA approval in 2000 for the treatment of hypogonadism, a condition that frequently causes mood, energy, and sexual dysfunctions, as well as a number of injury-related conditions like those suffered by severe burn and accident victims. AndroGel, a very popular form of testosterone, is sold all over the world under a few less well-known brand/trade names, most notably Testogel (produced in the UK by Laboratoires Besins and distributed by Bayer), Testim (produced in the US by Auxilium Pharmaceuticals, Inc.), and several generic variations frequently marketed as testosterone cream or gel.
The target body regions for testosterone cream’s transdermal delivery system are the same or very comparable to those for injections and other testosterone delivery methods. More specifically, testosterone cream absorbs best when applied to heavily muscled body parts, just like testosterone injections do. Since there are more testosterone-absorbing capillaries at the site of application when there is more muscle, testosterone can enter the bloodstream more quickly.”
“Sexual development occurs throughout life at all stages of development thanks to endogenous testosterone. It is made synthetically from cholesterol. Androgens play a significant part in the development of males from the time they are fetuses to adulthood. They are essential during puberty. Small amounts of testosterone are also secreted by females from their ovaries. Male sexuality cannot be sustained by the adrenal cortex’s androgen release.
Through a negative-feedback mechanism, elevated androgen plasma concentrations inhibit gonadotropin-releasing hormone (which lowers endogenous testosterone), luteinizing hormone, and follicle-stimulating hormone. Additionally, the production of erythropoietin, the balance of calcium, and blood sugar are all impacted by testosterone. Androgens have a high lipid solubility, which allows them to reach target tissue cells quickly. When testosterone enters cells, it is enzymatically converted to 5-alpha-dihydrotestosterone and joins with cystolic receptors to create a loosely bound complex. The steroid-receptor complex causes cellular alterations in the nucleus and the start of transcription, which are the causes of androgen activity.
RNA polymerase is often stimulated by endogenous androgens, which increases protein synthesis. The growth and maturation of the prostate, seminal vesicle, penis, and scrotum as well as other aspects of typical male sexual development are regulated by these proteins. Androgens promote a dramatic increase in muscle growth and development throughout puberty, as well as a redistribution of body fat. The larynx and vocal cords undergo changes as well, which deepen the voice. The development of the beard and the expansion of body hair mark the end of puberty. The androgens also control the fusion of the epiphyses, the cessation of growth, and the preservation of spermatogenesis. Exogenous androgens must be used in the absence of endogenous androgens to support normal male development and growth.”
Your doctor needs to know if you have any of the following conditions: breast cancer, sleep apnea, diabetes, heart disease, kidney disease, liver disease, lung disease, prostate cancer or enlargement, any unusual or allergic reactions to testosterone or other medications, being pregnant or trying to become pregnant, or breastfeeding. While using testosterone, your doctor will need to have frequent bloodwork taken. Most athletic organizations forbid using this drug on athletes.
Since topical gels and solutions are frequently flammable, using any topical gel or solution formulation of testosterone should be done without being exposed to fire, flame, or cigarette smoking.
Male patients with prostate cancer or breast cancer should not use testosterone since it can promote the formation of malignant tissue. Prostatic hypertrophy patients should be treated carefully because androgen therapy may exacerbate the condition’s signs and symptoms and raise the possibility of cancer developing. Prior to beginning testosterone replacement medication, elderly patients and other patients with clinical or demographic traits known to be linked to an elevated risk of prostate cancer should be assessed for the disease’s existence. Prostate cancer surveillance in patients receiving testosterone therapy ought to follow existing guidelines for eugonadal men. Age-related hypogonadism alone in geriatric patients or andropause are not advised for testosterone replacement therapy because there is inadequate evidence of its safety and effectiveness.[1] Furthermore, due to a dearth of elderly participants in controlled trials, the effectiveness and long-term safety of testosterone topical solution in patients older than 65 have not been established.[2] The Beers Criteria state that testosterone is a potentially inappropriate drug (PIM) for geriatric people and that it should be avoided since it may cause cardiac issues and is contraindicated in cases of prostate cancer. Use for moderate to severe hypogonadism is acceptable in the opinion of the Beers expert panel.[3]
Patients with liver disease or malfunction should be given testosterone with caution due to decreased drug clearance and an increased risk of drug buildup. Additionally, edema brought on by sodium and water retention may develop while taking androgens for treatment. In individuals with hepatic disease, renal disease such as nephritis and nephrosis, preexisting edema, or cardiac disease such as heart failure, coronary artery disease, and myocardial infarction (MI), use testosterone with caution as fluid retention may exacerbate these symptoms. Further, regardless of pre-existing heart disease, research is being done into the potential link between testosterone usage and an increased risk of serious cardiovascular events. Adult male patients with an average age of 60 were included in an observational study at the U.S. Veterans Affairs medical system. Retrospective analysis comprised patients (n = 8779) undergoing coronary angiography with a documented low blood testosterone levels of less than 300 ng/dl. Within the larger group, 1223 guys underwent testosterone therapy after a median of 531 days had passed since coronary angiography; 7486 males did not. In the three years following coronary angiography, individuals taking testosterone therapy experienced a serious and/or fatal cardiovascular event at a rate of 25,7% compared to patients not receiving therapy at a rate of 19,9%. (MI, stroke, death).[4] The incidence of acute non-fatal MI following a first testosterone prescription was examined in a second observational research (n = 55,593) in both younger (=55 years) and older (>=65 years) adult males. When compared to the incidence rate of MI happening in the year preceding the first testosterone prescription, the incidence rate of MI occurring 90 days after the first prescription was studied. There was a 2-fold increase in MI risk among older men during the 90-day window, and there was a 2- to 3-fold increase in MI risk among younger men with a history of cardiac disease. Younger men without a history of heart disease, in comparison, did not exhibit an elevated risk.[5] In response to these findings, the FDA said in the beginning of 2014 that it will look into any potential associations between testosterone therapy and serious cardiovascular events. The FDA has not determined that testosterone therapy permitted by the agency raises the risk of stroke, MI, or demise. But healthcare practitioners are recommended to carefully examine whether the potential dangers outweigh the expected benefits of treatment. When the review is over, the FDA will announce its final results and suggestions.[6]
In patients with apnea risk factors including obesity or chronic respiratory disease, testosterone esters therapy for hypogonadal males may make the condition worse. Additionally, it is unknown if testosterone topical solution and intranasal gel are safe and effective in treating obese men with BMIs greater than 35 kg/m2.[2][7]
Polycythemia is a danger for patients taking large doses of testosterone. Patients receiving testosterone should routinely have their hemoglobin and hematocrit levels checked to look for polycythemia.
Due to the potential harm it could cause to the developing fetus, testosterone is not recommended during pregnancy (FDA pregnancy risk category X). When getting testosterone therapy, women who are capable of having children should use reliable contraception. There should be no specific reason to provide the items to women during labor or obstetric delivery because testosterone is not utilized throughout pregnancy; safety and efficacy in these circumstances have not been shown.[2]
Testosterone is particularly contraindicated in females; the medication is intended for males; and the dosage type delivers more testosterone than should be advised for female patients in several endocrine circumstances.[8] Additionally, due to a lack of controlled studies and/or the possibility for virilizing effects, products under the Androgel, Androderm, Aveed, Fortesta, and Striant brands are not recommended for use in females.[9][10][11][12][13] Patients who are female and taking different types of testosterone therapy need to be properly watched for symptoms of virilization (deepening of the voice, hirsutism, acne, clitoromegaly, and menstrual irregularities). The concurrent use of estrogens does not prevent virilization, which occurs frequently at high levels. While some virilization may be deemed to be acceptable during treatment for breast cancer, medication therapy must be stopped if moderate virilism is visible in order to prevent long-term virilization.[1] Females should be informed that if they come into contact with a treated patient, they may unintentionally come into contact with some testosterone dose forms (i.e., ointments, solutions, and gels). In clinical tests, 15-minute periods of strong skin-to-skin contact with a female partner produced serum female testosterone levels > 2 times the female baseline values within 2—12 hours of gel application by male subjects. The transmission of testosterone to the female was prevented when garments covered the treatment spot on the male. Children who came into contact with the treatment site while being treated unintentionally became exposed to topical testosterone gel.The negative side effects mentioned include enlarged genitalia, pubic hair growth, advanced bone aging, increased libido, and aggressive conduct. When exposure to the substance was terminated, the majority of patients’ symptoms disappeared. The enlarged genitalia and advanced bone age did not fully revert to expected values in a small number of patients, nevertheless. The FDA advises taking safety measures to reduce the possibility of unintentional exposure to topical testosterone products, including washing hands with soap and warm water after each application, covering the application site with clothing, and removing the medication with the same precaution when it is anticipated that contact with another person will occur. The non-treated person should wash the area with soap and water as soon as possible if they come into direct contact with the location of testosterone application.[2]Testosterone topical solution, transdermal patches, and gels are contraindicated in lactating women who are breast-feeding.[2][9] It is recommended that other testosterone formulations be avoided during breast-feeding as well.[14][1] Uncertainty exists regarding the distribution of testosterone in breast milk and whether exposure would elevate levels above those typically present in human milk. Significant breast-feeding exposure to this androgen may have negative infant androgenic effects, and the medication may also prevent the mother from starting her milk supply properly.[15] Historically, testosterone/androgens have been used adjunctively for lactation suppression.[15] Alternative methods to breast-feeding are recommended in lactating women receiving testosterone therapy.
In patients with diabetes mellitus, androgen therapy—such as testosterone—should be administered with caution because it can lead to a loss of diabetic control. It is advised to closely check blood glucose levels.
In patients with hypercalcemia, which can be aggravated in those with metastatic breast cancer, testosterone has been shown to trigger osteolysis and should be administered with caution.
Anaphylactoid reactions as well as significant pulmonary oil microembolism (POME) reactions have been linked to the administration of testosterone undecanoate. During or right away following a 1000 mg intramuscular injection of testosterone undecanoate, incidences of POME responses have been reported. Coughing, the desire to cough, dyspnea, hyperhidrosis, throat constriction, chest pain, disorientation, and syncope were among the symptoms. However, some cases prolonged up to several hours and required emergency care and/or hospitalization. The majority of cases lasted a few minutes and were treated with supportive measures. Clinicians should take care to inject testosterone undecanoate deeply into the gluteal muscle and prevent intravascular injection. In addition to POME reactions, instances of anaphylaxis, including potentially fatal events, have also been documented after testosterone undecanoate injection intramuscularly. It is not advisable to provide testosterone undecanoate again to patients who may have experienced hypersensitive responses. Monitor the patient for 30 minutes following each administration, and in the event of severe POME or anaphylactoid reactions, administer the necessary medical care. The only way to obtain testosterone undecanoate (Aveed) is through a restricted program known as the Aveed REMS Program due to the possibility of serious POME and allergic reactions. Clinicians who want to order or dispense Aveed must be certified with the REMS Program in order to do so. Additionally, healthcare facilities must be REMS Program certified and have the resources to offer emergency medical care in cases of serious POME and anaphylaxis. Further information is available at www.AveedREMS.com or call 1—855—755—0494.[13]
Intranasal formulations of testosterone (e.g., Natesto) are not recommended for individuals with a history of nasal disorders such as nasal polyps; nasal septal perforation; nasal surgery; nasal trauma resulting in nasal fracture within the previous 6 months or nasal fracture that caused a deviated anterior nasal septum; sinus surgery or sinus disease. In addition, the safety and efficacy of intranasal testosterone has not been evaluated in individuals with mucosal inflammatory disorders such as Sjogren’s syndrome. Patients with rhinorrhea (rhinitis) who are receiving intranasal formulations of testosterone may experience decreased medication absorption secondary to nasal discharge. These patients may experience a blunted or impeded response to the intranasal medication. In clinical evaluation, serum total testosterone concentrations were decreased by 21—24% in males with symptomatic allergic rhinitis, whether treated with nasal decongestants or left untreated. Treatment with intranasal testosterone should be delayed until symptoms resolve in patients with nasal congestion, allergic rhinitis, or upper respiratory infection. If severe rhinitis symptoms persist, an alternative testosterone replacement therapy is advised.[7]
The safety and efficacy of testosterone topical products Androgel, Axiron, Fortesta, and Testim as well as Striant buccal tablets, Natesto intranasal gel, and Aveed injectable testosterone undecenoate have not been established in neonates, infants, children, and adolescents < 18 years old.[10][2][16][11][12][13][7] In addition, the safety and efficacy Depo-Testosterone injection has not be established in children < 12 years,[14] and Androdem patches have not been evaluated in pediatric patients < 15 years.[9] In general, using testosterone in youngsters should only be done with the utmost caution. Testosterone can hasten bone maturation without promoting linear growth to make up for it, which can sometimes limit adult stature. In order to monitor the rate of bone maturation and the impact of the medication on epiphyseal centers in prepubertal males receiving testosterone, radiographic exams of the hand and wrist should be carried out every six months. Growth stops once the epiphyses have closed. Epiphyseal closure can be increased for several months even after the end of the treatment. Pediatric patients have also unintentionally come into contact with topical testosterone gel after being treated persons had applied it directly to their skin. The negative side effects mentioned include enlarged genitalia, pubic hair growth, advanced bone aging, increased libido, and aggressive conduct. When exposure to the substance was terminated, the majority of patients' symptoms disappeared. The enlarged genitalia and advanced bone age did not fully revert to expected values in a small number of patients, nevertheless. The FDA advises taking safety measures to reduce the possibility of inadvertent exposure, including covering the application location with clothing, removing the drug with soap and water when coming into touch with another person, and washing hands with soap and warm water after each application. The non-treated person should wash the area with soap and water as soon as possible if they come into direct contact with the location of testosterone application.
“Some diabetes medications, some drugs to treat or prevent blood clots including warfarin, oxyphenbutazone, propranolol, and steroid drugs like prednisone or cortisone are examples of possible interactions. It’s probable that not all combinations are covered by this list.
NOTE: Testosterone is a substrate for hepatic cytochrome P450 (CYP) 3A4 isoenzyme.[17] Testosterone is also both transported by and an inhibitor of P-glycoprotein transport.[18]
Warfarin’s anticoagulant effect can be enhanced by testosterone.[19] With this drug-drug interaction, some individuals have experienced serious bleeding. The mechanism by which testosterone reduces procoagulant factors is unknown. If testosterone therapy is also taken, it might be required to lower the dose of warfarin. It is advised to monitor INR and prothrombin time more often in patients using these oral anticoagulants, particularly at the beginning and end of androgen therapy.[9] It is unclear if testosterone can augment the anticoagulant response to heparin therapy or if testosterone alters the effect of other non-coumarin oral anticoagulants in a similar manner.
Androgens may raise plasma concentrations of cyclosporine, increasing the risk of nephrotoxicity, according to case reports with methyltestosterone and danazol.[20][21][22][23]
Testosterone and corticosteroid co-administration may raise the risk of edema, particularly in patients with underlying liver or heart illness. Fludrocortisone, a corticosteroid with higher mineralocorticoid action, may be more prone to result in edema. administer these medications with caution and in combination.[24]
Goserelin and leuprolide inhibit steroidogenesis.[25][26] Concomitant use of androgens with goserelin or leuprolide is relatively contraindicated and would defeat the purpose of goserelin or leuprolide therapy.
Androgens should be provided concurrently with other hepatotoxic drugs with caution because they can enhance the risk of hepatotoxicity. Particularly for those with a history of liver illness, patients should be constantly watched for symptoms of liver damage.
Androgens might be required to help with the human growth hormone response to growth, however in prepubescent males, high androgen dosages can hasten epiphyseal maturation.[27]
Androgens are known to stimulate erythropoiesis.[28] Despite the fact that endogenous generation of erythropoietin is depressed in patients with chronic renal failure, other tissues besides the kidney can synthesize erythropoietin, albeit in small amounts. Concurrent administration of androgens can increase the patient’s response to epoetin alfa, reducing the amount required to treat anemia. Because adverse reactions have been associated with an abrupt increase in blood viscosity, this drug combination should be avoided, if possible. Further evaluation of this combination needs to be made.
It would be nonsensical for patients taking androgens to utilize these antiandrogenic medications because the 5-alpha reductase inhibitors (such as dutasteride and finasteride) have antiandrogenic effects that are antagonistic to the actions of androgens.[29][30]
Serenoa repens and saw palmetto have not been formally researched or reported for drug interactions. Extracts from saw palmetto seem to have antiandrogenic properties.[31][32] The antiandrogenic effects of Saw palmetto, Serenoa repens would be expected to antagonize the actions of androgens; it would seem illogical for patients taking androgens to use this herbal supplement.
There is some evidence that testosterone levels rise when fluconazole is administered. Fluconazole dosages of 200 mg/day or above seem to have a higher likelihood of having this effect than those of 25–50 mg/day.[33] The clinical significance of this interaction is unclear at this time. Although data are not available, a similar reaction may occur with voriconazole. Both fluconazole and voriconazole are inhibitors of CYP3A4, the hepatic microsomal isoenzyme responsible for metabolism of testosterone.[34]
In patients with diabetes mellitus, exogenously administered androgens (such as anabolic steroids or testosterone derivatives) have varying effects on blood glucose management. In general, insulin resistance is linked to decreased testosterone levels. Furthermore, when exogenous androgens are given to hypogonadal males (with or without diabetes), glycemic control often improves as seen by significantly lower fasting plasma glucose and HbA1c levels. In one study, testosterone undecenoate 120 mg PO/day for three months reduced HbA1c levels from a baseline of 10.4% to 8.6% (p 0.05), while fasting plasma glucose levels dropped from a baseline of 8 mmol/l to 6 mmol/l (p 0.05). The HbA1c and fasting plasma glucose concentrations did not significantly decrease in participants consuming the placebo.[35] Similar results have been demonstrated with intramuscular testosterone 200 mg administered every 2 weeks for 3 months in hypogonadal men with diabetes.[36] In healthy men, testosterone enanthate 300 mg IM/week for 6 weeks or nandrolone 300 mg/week IM for 6 weeks did not adversely affect glycemic control; however, nandrolone improved non-insulin mediated glucose disposal.[37] It should be noted that some studies have shown that testosterone supplementation in hypogonadal men has no effect on glycemic control.[38][39] On the other hand, giving powerlifters high dosages of anabolic steroids reduced their ability to tolerate glucose, maybe by causing insulin resistance.[40] Regardless of endogenous testosterone levels, it would be important to follow all type 2 diabetes patients taking anti-diabetic medications who receive androgens for changes in glycemic control despite conflicting results. If either hypo- or hyperglycemia develops, the dosage of the anti-diabetic medication may need to be adjusted.
Both genistein and daidzein inhibit the enzyme 5 alpha-reductase isoenzyme II in vitro, which reduces the conversion of testosterone to the powerful androgen 5-alpha-dihydrotestosterone (DHT) and, consequently, the proliferation of tissues that depend on testosterone. [41] Although it is believed to be less effective, the activity is comparable to that of finasteride. The soy isoflavones may theoretically counteract the activity of the androgens because they seem to inhibit type II 5-alpha-reductase.
Although it is believed to be less effective, the activity is comparable to that of finasteride. The soy isoflavones may theoretically counteract the activity of the androgens because they seem to inhibit type II 5-alpha-reductase. [34] The clinical significance of this theoretical interaction is not known.
A P-glycoprotein transport inhibitor is testosterone.[34] Ranolazine is a substrate of P-glycoprotein, and inhibitors of P-glycoprotein may increase the absorption of ranolazine.[42] In addition, ranolazine inhibits CYP3A and may increase plasma concentrations of drugs that are primarily metabolized by CYP3A4 such as testosterone.[34]
Ambrisentan is a substrate for P-glycoprotein transport, an energy-dependent drug efflux pump.[43] The inhibition of P-glycoprotein, by drugs such as testosterone,may lead to a decrease in the intestinal metabolism and an increase in the oral absorption of ambrisentan.[34] If ambrisentan is coadministered with a P-glycoprotein inhibitor, patients should be monitored closely for adverse effects.
Coadministration of oxyphenbutazone and testosterone may lead to elevated concentrations of oxyphenbutazone. Monitor patients for adverse effects when coadministering these drugs together.[24]
Testosterone cypionate has been shown to increase the clearance of propranolol in one study. Monitor patients taking testosterone and propranolol together for decreased therapeutic efficacy of propranolol.[24]
When dabigatran and testosterone are taken together, the serum concentration of dabigatran may rise, increasing the risk of side effects. Dabigatran and testosterone shouldn’t be administered at the same time to patients who have significant renal impairment (CrCl 15–30 ml/min). While testosterone is a P-gp inhibitor, dabigatran is a P-gp substrate.[18] P-gp inhibition and renal impairment are the major independent factors that result in increased exposure to dabigatran.[44]
Concomitant use of testosterone, a P-glycoprotein (P-gp) inhibitor,[18] and afatinib, a P-gp substrate, may increase the exposure of afatinib. If the use of both agents is necessary, consider reducing the afatinib dose if the original dose is not tolerated.[45]
Concomitant use of intranasal testosterone (e.g., Natesto) and other intranasally administered drugs in not recommended; the drug interaction potential between these agents is unknown.[7] Eighteen males with seasonal allergic rhinitis were treated with intranasal testosterone and randomized to receive oxymetazoline (30 minutes prior to intranasal testosterone) or no treatment. In general, serum total testosterone concentrations were decreased by 21—24% in males with symptomatic allergic rhinitis, due to the underlying condition. A mean decrease in AUC and Cmax (2.6% and 3.6%, respectively) for total testosterone was observed in males with symptomatic seasonal rhinitis when treated with oxymetazoline compared to untreated patients. Concomitant use of oxymetazoline does not impact the absorption of testosterone.[7]
This list may not include all possible interactions. Give your health care provider a list of all the medicines, herbs, non-prescription drugs, or dietary supplements you use. Also tell them if you smoke, drink alcohol, or use illegal drugs. Some items may interact with your medicine.”
“During extended testosterone therapy, male patients may undergo feminization, which is thought to be caused by the suppression of gonadotropin secretion and the conversion of androgens to estrogens. Mastalgia and gynecomastia are two of these symptoms, which are particularly pronounced in male patients with concurrent hepatic illness. Gynecomastia (Testim: 1 percent; Androgel: 1–3 percent) and mastalgia (Androgel: 1–3 percent) were reported during a clinical evaluation of testosterone gel. [10][16] Less than 1% of patients on Axiron reported experiencing mastalgia and higher blood testosterone levels.[2] Feminizing effects of testosterone are generally reversible. During exogenous administration of androgens, endogenous testosterone release is inhibited through feedback inhibition of pituitary luteinizing hormone (LH). At large doses of exogenous androgens, spermatogenesis inhibition may occur through feedback inhibition of pituitary follicle stimulating hormone (FSH).[2][13] Similar to other testosterone therapies, decreased serum testosterone and oligospermia have been reported during post approval surveillance of testosterone topical gel.[10][12]
Both an increase and a decrease in libido may result with testosterone therapy. [13] In clinical evaluation of testosterone gel (Androgel), libido decrease was reported in 1—3% of patients.[10] Males in their senior years are more likely to experience priapism and excessive sexual excitement as a result of taking too much testosterone. One percent of individuals receiving Testim 50 or 100 mg daily reported experiencing spontaneous penile erections.[16] During post approval experience with testosterone topical gel (Fortesta), priapism as well as impotence (erectile dysfunction) were reported.[12]
Long-term testosterone therapy can cause prostatic enlargement, and older male patients are more likely to have these side effects. One percent of 205 patients using the testosterone gel Testim 50 or 100 mg daily were found to have benign prostatic hyperplasia, or BPH. [16] Clinical trials for testosterone patch (Androderm) include reports of unspecified prostate abnormalities in 5% of patients.[9] Less than 1% of people on Axiron had a recorded case of prostate cancer.2 In addition, increases in serum PSA concentrations have been reported in clinical trials for testosterone topical solution (Axiron: 1—4%), topical gel (Fortesta: 1.3%), and intranasal gel (Natesto: 5.1—5.8%).[2][12][7] In a 180 Day, Phase 3 study of testosterone gel (Androgel), prostate disorder (3—5%) including enlarged prostate, BPH, and elevated PSA were reported; testis disorder (1.9—3%) including left varicocele and slight testicular sensitivity were also reported. In 162 hypogonadal men receiving testosterone gel (Androgel) during a 3-year open-label extension trial, increases in serum PSA concentrations (defined as >= 2x baseline concentrations or any single absolute value >= 6 ng/ml) were seen in approximately 18% of patients (n = 29). The majority of these increases were seen in the first year of therapy (23/29 or 79%). Four patients had a single value >= 6 ng/ml: 2 of these patients had prostate cancer detected upon biopsy. In the same study population, enlarged prostate and urinary symptoms including nocturia, urinary hesitancy, urinary incontinence, urinary retention, urinary urgency and weak urinary stream were also reported. Finally, 1 patient reported prostate disorder requiring a transurethral resection of the prostate (TURP) considered possibly related to treatment by investigators.[10] Dysuria and hematuria have also been reported during postmarketing surveillance of testosterone therapy. Hematuria (< 3%), prostatitis (< 3%), and polyuria (< 3%) have been reported in patients receiving Androderm.[9] In patients receiving testosterone therapy, surveillance for prostate cancer (as a secondary malignancy) should be consistent with current practices for eugonadal men. Signs of acute epididymitis (e.g., pyrexia, pain in the inguinal region) and/or urinary urgency should prompt withdrawal of the drug and reevaluation of dosage. When androgens are administered to females, virilization—which can show as acne, the development of facial hair or an excessive amount of body hair (hirsutism), an enlarged clitoris, smaller breasts, and a deeper voice—can take place. When these symptoms first start, if testosterone therapy is stopped, they typically go away. Hirsutism was among the dermatological effects that were documented after approval or in less than 1% of individuals who used testosterone gel. Long-term treatment should be weighed against the risk because it can result in permanent masculinity.[10][6][13] Disruption of the regular menstrual cycle secondary to testosterone-induced suppression of gonadotropin secretion can lead to amenorrhea or oligomenorrhea.[10][6] Testosterone is linked to teratogenesis and could harm an unborn child. A fetus's (male or female) exposure to androgens may virilize them to varied degrees. The transmission of topical testosterone from male to female partners is one way that should be avoided during pregnancy. Skin responses at the application site are linked to topical testosterone products. Transient mild to moderate erythema was seen at the site of application in the majority of individuals throughout therapy in clinical tests with the testosterone patch (Androderm). Application site reactions of any type were reported 28 percent of the time overall (10 subjects with 13 adverse reactions). Adverse reactions at the application site have been reported as pruritus (17–37%), burn-like blister reaction under the system (12%), erythema ( 7%), exfoliation ( 3%) and vesicular rash (6%) as well as allergic contact dermatitis to the system (4%) and burning (3%) and induration (3%) and a general rash (unspecified) (2%) Bullous rash, skin necrosis, or the emergence of a skin ulcer are occasionally associated with blisters that were recorded during trails. The majority of lesions were discovered in situations where the patch was applied on bony prominences or over areas of the body that may have experienced prolonged pressure while lying or sitting. Other dermatological reactions at the application site that happen in less than 1% of patients include contamination, mechanical irritation, bullous rash, and rash (unspecified). 5% of patients stopped receiving treatment because of chronic skin discomfort. After removing the transdermal device, the afflicted area can be treated with an over-the-counter topical hydrocortisone lotion to reduce mild skin irritation.[9] Dermatological reactions seen during testosterone topical solution (Axiron) clinical trials include: application site skin irritation (7—8%), erythema (5—7%), and folliculitis (< 1%).[2] Other less common adverse reactions include: general erythema (< 1%) and application site edema and warmth (reported in at least 2 patients).[2] Application site reactions have also been reported for testosterone gel (Fortesta: 16.1%; Androgel: 3—5.6%; Testim: 2—4%). Other dermatological reactions reported during clinical trials with testosterone gel (Androgel) include: xerosis (1.9%), acne (1—8%), and pruritis (1.9%). Contact dermatitis was reported in 2.1% of patients treated with testosterone gel (Androgel 1.62%).[46] All testosterone therapy influences the growth and secretion of the sebaceous glands, which can cause seborrhea and acne indistinguishable from acne vulgaris.[9] Acne vulgaris (> 1%) was reported in a clinical evaluation of testosterone solution (Axiron).[2] Alopecia resembling male pattern baldness has also occurred in patients receiving long-term therapy or excessive testosterone doses. Dermatologic reactions reported post-approval or in < 1% of patients using testosterone gel, regardless of brand, include: acne, allergic dermatitis, diaphoresis, alopecia, erythema, hair discoloration, maculopapular rash, paresthesias, pruritus, rash (unspecified), skin irritation, swelling, and xerosis.[10][16][12] During clinical evaluation and post marketing surveillance, hyperhidrosis (1.3%) was reported among patients receiving testosterone undecanoate.[13] The testosterone buccal mucoadhesive system has been linked to dental pain, including gum or mouth irritation (9.2%), dysgeusia (4.1%), gum pain (3.1%), gum soreness (3.1%), gum edema (2%) and taste distortion (dysgeusia, 2 percent ). The majority of gum-related adverse events were brief; gum soreness and irritation typically subsided within 1–8 days and 1–14 days, respectively. During clinical trials, 1 patient experienced buccal mucosal roughening, gingivitis, gum blisters, nose edema, lip stinging, and toothache.[11] Dysgeusia (reported as taste disorder) was reported in 1% of patients receiving testosterone gel (Testim) and judged possibly, probably, or definitely related to the study drug.[16] However, other topical or injectable testosterone medications have not been associated with dysgeusia as a side effect, and systemic and topically applied testosterone are not known to frequently induce taste disruption.[47] In pre-pubertal males, early exposure to pharmaceutical amounts of testosterone or other androgens can cause virilism, which can be harmful because it is accompanied by an early closure of the epiphysis. Growth stops once the epiphyses have closed. Monitoring the development of the skeleton should be done every six months or so. Growth stops once the epiphyses have closed. Epiphyseal closure can be improved for several months even after stopping testosterone therapy.[10] Retention of salt, chloride, water, potassium, and inorganic phosphates has been linked to androgen therapy.[6][13] Weight gain may be a symptom of peripheral edema, which can develop as a result of increased fluid retention in conjunction with sodium chloride. These effects could be more noticeable in the beginning of androgen therapy. Only a minor degree of fluid retention happens when hypogonadism is treated with standard therapeutic testosterone levels. The fluid retention is more important when treating individuals with congestive heart failure or poor renal function.[10] In animal models, testosterone has been shown to elevate blood pressure, change naturesis, cause vasoconstriction, and stimulate the renin-angiotensin-aldosterone pathway. As a result, androgens may alter blood pressure; nevertheless, it is still unknown how testosterone regulates blood pressure. During the clinical evaluation and post-approval monitoring of testosterone therapy, hypertension has been noted. 2.1–3% of patients taking testosterone gel (Androgel) in clinical studies complained of hypertension.[10][46] Hypertension (1%) as well as decreased diastolic pressure (1%) were reported in trials involving testosterone gel (Testim).[16] Hypertension (>1%) was reported in patients using testosterone topical solution (Axiron).[2] Androgens may influence the prevalence of cardiovascular disease in addition to blood pressure. Investigations are now being conducted to determine whether testosterone usage, regardless of pre-existing cardiac illness, is associated with an increased risk of serious cardiovascular events. Adult male patients with an average age of 60 were included in an observational study at the U.S. Veterans Affairs medical system. Retrospective analysis comprised patients (n = 8779) undergoing coronary angiography with a documented low blood testosterone levels of less than 300 ng/dl. Within the larger group, 1223 guys underwent testosterone therapy after a median of 531 days had passed since coronary angiography; 7486 males did not. In the three years following coronary angiography, individuals taking testosterone therapy experienced a serious and/or fatal cardiovascular event at a rate of 25,7% compared to patients not receiving therapy at a rate of 19,9%. (myocardial infarction, stroke, death). [4] A second observational study, investigated the incidence of acute non-fatal myocardial infarction (MI) following an initial testosterone prescription in both younger (<= 55 years) and older (>= 65 years) adult males (n = 55,593). The incidence rate of MI occurring within 90 days following the initial testosterone prescription was compared to the incidence rate of MI occurring in the one year leading-up to the first prescription. Among older males, a 2-fold increase in the risk of MI was observed within the 90 day window; among younger males with a pre-existing history of cardiac disease, a 2- to 3-fold increased risk of MI was observed. In contrast, no increased risk was observed in younger males without a history of cardiac disease.[5] In response to these findings, the FDA said in the beginning of 2014 that it will look into any potential associations between testosterone therapy and serious cardiovascular events. The FDA has not determined that testosterone therapy permitted by the agency raises the risk of stroke, MI, or demise. But healthcare practitioners are recommended to carefully examine whether the potential dangers outweigh the expected benefits of treatment. When the review is over, the FDA will announce its final results and suggestions.[6]
Certain androgens can cause hepatic dysfunction, hence it is advisable to monitor liver function tests on a regular basis.[4][6] As opposed to overt jaundice or other liver problems, which are uncommon with testosterone use in general, increased hepatic enzymes are more likely to occur with use as advised. Administration of 17-alpha-alkylating hormones (like methyltestosterone) or abuse of such androgenic hormones by athletes are more likely to have negative effects on the liver. Abuse of these hormones causes liver changes consistent with fatty liver disease (steatosis) in an estimated 2.4 percent of people, even in the absence of other risk factors for fatty liver. If cholestatic jaundice, hepatitis, or another serious liver malfunction occurs, testosterone should be stopped. Hepatic neoplasms and periosis hepatis are uncommon, but when they do develop, they can be fatal.[10]
Numerous testosterone therapy trials have observed headache; regardless of formulation, incidence rates of headache range from 1 to 6 percent. A few instances of mood changes, such as emotional lability ( 3%), bewilderment ( 1%), despair ( 3%), nervousness ( 3%), anxiety (> 1%), rage (> 1%), asthenia ( 1%), hostility ( 1%), and mood swings ( 1%), have also been noted in several testosterone investigations. [2] Abnormal dreams (Fortesta: 1.3%) and insomnia (Testim: 1%) have been reported in patients receiving testosterone gel.1612 Hot flashes or flushing (Testim: 1%) and asthenia (Androgel: 1—3%) were also reported for patients receiving testosterone.[16][10] Diarrhea (3—4%) and vomiting (3—4%) have been reported among patients receiving testosterone solution (Axiron).[2] Diarrhea (< 3%), gastroesophageal reflux disease (< 3%), back pain (6%), chills (< 3%), fatigue (< 3%) have been reported in patients receiving Androderm transdermal patch.[9] Miscellaneous adverse reactions reported post-approval or in < 1% of patients using exogenous testosterone, regardless of formulation include: abdominal pain (cramps), abnormal renal function, appetite stimulation, asthma, dizziness, hyperglycemia, increased lacrimation, malaise, nausea, pain in extremity (musculoskeletal pain), pelvic pain, and vitreous detachment. Other miscellaneous reactions reported during post approval surveillance of testosterone undecenoate include: sudden hearing loss, tinnitus, and myalgia.[13] The effects of testosterone therapy can worsen hypercalcemia and promote osteolysis. Patients who are bedridden or who have metastatic breast cancer are more likely to develop androgen-induced hypercalcemia. [10] Skeletal adverse reactions reported during post approval surveillance of testosterone undecanoate included osteopenia and osteoporosis.[13] Hypercholesterolemia and hypertriglyceridemia are two unfavorable alterations in serum lipid profiles that can be brought on by testosterone. Throughout treatment, regular lipid profile monitoring may be desirable.[13] Observational research on post-menopausal women, bodybuilders, and weightlifters who used anabolic steroids found 'pro-atherogenic' changes in their lipid profiles, including a drop in HDL levels and an increase in LDL levels. The ratio of HDL-C to LDL-C may be decreased more by synthetic androgens than by testosterone. Although there is uncertainty regarding the effects of androgen-induced hypercholesterolemia, attention should be taken, especially in those who are susceptible to dyslipidemia or atherosclerosis. Individualize treatment if major lipid changes necessitate changing the dosage of testosterone or cholesterol-lowering medications or stopping testosterone treatment altogether. [10][13] The synthesis of erythropoietin is stimulated by testosterone. Increased erythropoiesis, particularly in females, can result in secondary polycythemia and accompanying consequences, such as erythrocytosis, which can cause headaches, weariness, dizziness, and irregular bleeding as well as skin redness and flushing. Polycythemia is a danger for patients taking large doses of testosterone. Increases in red blood cell count ( 1%), hematocrit (4–7%%), and hemoglobin (> 1%) were observed in clinical tests with testosterone solution (Axiron).[2] In studies of testosterone gel (Testim), patients receiving a 100 mg dose had clinically notable increases in both hematocrit (2.8%) and hemoglobin (2.3%).[16] Likewise, 2.1% of patients treated with testosterone gel (Androgel 1.62%) reported increased hematocrit or hemoglobin. In intranasal testosterone gel analysis, 4 of 306 exposed patients developed a hematocrit level > 55% (baseline: 48—51%; did not exceed 58%).[7] Therefore, periodic hemoglobin and hematocrit determinations should be considered in patients receiving long-term testosterone therapy. In general, testosterone therapy has been associated with suppression of clotting factors II, V, VII, and X and bleeding in patients on concomitant anticoagulant therapy.[6] GI bleeding was reported in 2% of patients receiving testosterone patch (Androderm) therapy during clinical evaluation. Hemarthrosis (< 3%) has also been reported Androderm.[9] During postmarketing surveillance of testosterone gel (Testim), prolonged aPPT and PT and prolonged bleeding time were reported.[16] Anemia was reported in 2.5% of patients receiving testosterone gel (Androgel) during clinical evaluation.[10] An increased risk of deep vein thrombosis (DVT) and acute pulmonary embolism (PE) is associated with testosterone use; events have been reported during post-marketing surveillance. Discontinue treatment with testosterone in patients reporting pain, swelling, warmth, and redness in the leg (DVT) or chest pain, trouble breathing, and cough (PE) and examine for possible VTE.[7][12] Other miscellaneous reactions reported during post approval surveillance of testosterone undecenoate include: thrombocytopenia, hyperparathyroidism, and hypoglycemia.[13] Anabolic steroids used intramuscularly may result in erythema, urticaria, post-injection discomfort, induration, and furunculosis. At the location of the testosterone implant pellets' implantation, inflammation and pain are likely. Additionally, testosterone pellets may slough off from the site of insertion. This usually happens as a result of shallow implantation or aseptic approach. You should keep an eye on the patients for any indications of an injection site reaction.[6][13] There haven't been many examples of anaphylactoid responses linked to oral and injectable testosterone therapy.[9][6] The use of testosterone undecanoate has been linked to anaphylactic and significant pulmonary oil microembolism (POME) reactions as well as pulmonary embolism instances. During or right away following a 1000 mg intramuscular injection of testosterone undecanoate, incidences of POME responses have been reported. Coughing, the desire to cough, dyspnea, hyperhidrosis, throat constriction (acute bronchospasm), chest pain, lightheadedness, and syncope were among the symptoms. However, some cases prolonged up to several hours and required emergency care and/or hospitalization. The majority of cases lasted a few minutes and were treated with supportive measures. In addition to POME reactions, instances of anaphylaxis, including potentially fatal events, have also been documented after testosterone undecanoate injection intramuscularly. [13] The only way to obtain testosterone undecanoate (Aveed) is through a restricted program known as the Aveed REMS Program due to the possibility of serious POME and allergic reactions. Clinicians who want to order or dispense Aveed must be certified with the REMS Program in order to do so. Additionally, healthcare facilities must be REMS Program certified and have the resources to offer emergency medical care in cases of serious POME and anaphylaxis. Further information is available at www.AveedREMS.com or call 1—855—755—0494.[13] During post-marketing surveillance, transient respiratory responses have been noted. These include the need to cough, coughing fits, and respiratory discomfort right away after intramuscular testosterone enanthate injection. It is important to ensure that testosterone preparations are injected slowly and deeply into the gluteal muscle.6 Nasopharyngitis or pharyngitis (> 1 %) was reported in patients receiving testosterone topical solution (Axiron).[2]
In individuals with sleep apnea risk factors, such as obesity or chronic lung disease, testosterone therapy for hypogonadal males may raise the risk of developing sleep apnea.[10][13]
The following nasal side effects were among the most frequent adverse events in clinical studies of intranasal testosterone gel: nasopharyngitis (3.8–8.7% percent), rhinorrhea (3.8–7.8%), parosmia (5.8%), epistaxis (3.8–6.5%), nasal irritation or discomfort (3.8–5.9 percent), nasal scabbing (3.8–5.8 percent), nasal dryness (4.2 percent), nasal congestion (3.9 percent), and procedural pain (4.3 percent ). Long-term data on nasal safety are scarce, despite the fact that the majority of nasal complaints were mild or moderate in severity. Encourage patients to disclose any uncomfortable nose symptoms; if any exist, decide if they call for additional testing or ongoing care. Other respiratory side effects include sinusitis (3.8–4.3%), bronchitis (3.8–4.3%), and upper respiratory tract infections (3.8–4.3%). (3.8 percent ).[7]
Call your health care provider immediately if you are experiencing any signs of an allergic reaction: skin rash, itching or hives, swelling of the face, lips, or tongue, blue tint to skin, chest tightness, pain, difficulty breathing, wheezing, dizziness, red, swollen painful area on the leg.”
Due to the potential harm it could cause to the developing fetus, testosterone is not recommended during pregnancy (FDA pregnancy risk category X). When getting testosterone therapy, women who are capable of having children should use reliable contraception. There should be no specific reason to provide the items to women during labor or obstetric delivery because testosterone is not utilized throughout pregnancy; safety and efficacy in these circumstances have not been shown.[2]
The use of testosterone topical solutions, transdermal patches, and gels in nursing mothers is not advised.[2][9] It is advised to stay away from other testosterone formulations during nursing as well.[14][6] Uncertainty exists regarding the distribution of testosterone in breastmilk and whether exposure would rise above amounts typically present in human milk. Significant breastfeeding exposure to this androgen may have negative infant androgenic effects, and the medication may also prevent the mother from starting her milk supply properly.[15] Historically, testosterone/androgens have been used adjunctively for lactation suppression.[15] Alternative methods to breastfeeding are recommended in lactating women receiving testosterone therapy.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
- “1.DELATESTRYL (Testosterone Enanthate Injection, USP) package insert. Lexington, MA: Indevus Pharmaceuticals, Inc.; 2007 July.
- Axiron (testosterone) topical solution, package insert. Indianapolis, IN: Lilly USA, LLC; 2011 Dec.
- The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012;60:616-31.
- Vigen R, O’Donnell CI, Baron AE, et al. Association of testosterone therapy with mortality, myocardial infarction, and stroke in men with low testosterone levels. JAMA. 2013;310:1829-1836.
- WD Finkle, S Greenland, GK Ridgeway, et al. Increased Risk of Non-Fatal Myocardial Infarction Following Testosterone Therapy Prescription in Men. DOI: 10.1371/journal.pone.0085805
- FDA Medwatch – FDA evaluating risk of stroke, heart attack and death with FDA-approved testosterone products. Retrieved January 31, 2014. Available on the World Wide Web https://www.fda.gov/Drugs/DrugSafety/ucm383904.htm
- Natesto (testosterone) nasal gel package insert. Durants, Christ Church Barbados: Trimel BioPharma SRL; 2014 May.
- (testosterone gel) package insert. Malvern, PA: Auxilium Pharmaceuticals, Inc.; 2010 Apr.
- Androderm (testosterone transdermal system) package insert. Corona, CA: Watson Pharma, Inc.; 2014 Jun.
- Androgel (testosterone gel) package insert. Marietta, GA: Solvay Pharmaceuticals, Inc.; 2012 Sept.
- Striant (testosterone buccal system) package insert. Livingston, NJ: Columbia Laboratories, Inc.; 2014 Mar.
- Fortesta (testosterone) gel, package insert. Chadds Ford, PA: Endo Pharmaceuticals Inc.; 2010 Dec.
- Aveed (testosterone undecanoate Injection) package insert. Malvern, PA: Endo Pharmaceuticals Solutions Inc.; 2014 Mar.
- DEPO-TESTOSTERONE (testosterone cypionate) injection, package insert. New York, NY: Pharmacia & Upjohn Co.; 2006 Sept.
- Kochenour NK. Lactation suppression. Clin Obstet Gynecol. 1980;23:1045-1059.
- Testim (testosterone gel) package insert. Malvern, PA: Auxilium Pharmaceuticals, Inc.; 2010 Apr.
- Krauser JA, Guengerich FP. Cytochrome P450 3A4-catalyzed testosterone 6beta-hydroxylation stereochemistry, kinetic deuterium isotope effects, and rate-limiting steps. J Biol Chem 2005;280:19496—506.
- Barnes KM, Dickstein B, Cutler GB Jr, et al. Steroid transport, accumulation, and antagonism of P-glycoprotein in multidrug-resistant cells. Biochemistry 1996;35:4820—7.
- Wells PS, Holbrook AM, Crowther NR et al. Interaction of warfarin with drugs and food. Ann Intern Med 1994;121:676—83.
- Goffin E, Pirson Y, Geubel A, et al. Cyclosporine-methyltestosterone interaction. Nephron 1991;59:174—5.
- Borras-Blasco J, Rosique-Robles JD, Peris-Marti J, et al. Possible cyclosporin-danazol interaction in a patient with aplastic anaemia. Am J Hematol 1999;62:63—4.
- Moller BB, Ekelund B. Toxicity of cyclosporine during treatment with androgens. N Engl J Med 1985;313:1416.
- Ross WB, Roberts D, Griffin PJ, et al. Cyclosporin interaction with danazol and norethisterone. Lancet 1986;1:330.
- Androgel® (testosterone gel) package insert. Montrogue, France: Laboratories Besins International; 2005 Aug.
- Zoladex® (goserelin acetate) package insert. Wilmington, DE: AstraZeneca Pharmaceuticals LP; 2003 Dec.
- Viadur® (leuprolide implant) package insert. Westhaven, CT: Bayer Pharmaceuticals; 2002 May.
- Humatrope™ (somatropin);package insert. Indianapolis, IN: Eli Lilly and Company; 2003 Jul.
- Androderm® (testosterone transdermal system) package insert. Corona, CA: Watson Pharma, Inc.; 1999 Jan.
- Propecia® (finasteride) package insert. Whitehouse Station, NJ: Merck & Co., INC.; 2003 Oct.
- Avodart™ (dutasteride) package insert. Research Triangle Park, NC: GlaxoSmithKline; 2005 May.
- Robbers JE, Tyler VE. Tyler’s Herbs of Choice: the Therapeutic Use of Phytomedicinals. Binghamton NY: Haworth Herbal Press, Inc.; 1999.
- German Commission E. Saw Palmetto berry, Sabal fructus, monograph Published March 2, 1989 and revised January 17, 1991. In: Blumenthal, M et al ., eds. The complete German Commission E Monographs -Therapeutic Guide to Alternative Medicines. Bosto
- Lazar JD, Wilner KD. Drug interactions with fluconazole. Rev Infect Dis 1990;12:S327—33.
- Hansten P, Horn J. The Top 100 Drug Interactions: A Guide to Patient Management. includes table of CYP450 and drug transporter substrates and modifiers (appendices). H & H Publications, LLP 2014 edition.
- Boyanov MA, Boneva Z, Christov VG. Testosterone supplementation in men with type 2 diabetes, visceral obesity, and partial androgen deficiency. Aging Male 2003;6:1—7.
- Kapoor D, Goodwin E, Channer KS, et al. Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity, and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Clin Endocrinol 2006; 154:899—90
- Hobbs CJ, Jones RE, Plymate SR. Nandrolone, a 19-nortestosterone, enhances insulin-independent glucose uptake in normal men. J Clin Endocrinol Metab 1996; 81:1582—5.
- Corrales JJ, Burgo RM, Garcia-Berrocal B, et al. Partial androgen deficiency in aging type 2 diabetic men and its relationship to glycemic control. Metabolism 2004;53:666—72
- Lee CH, Kuo SW, Hung YJ, et al. The effect of testosterone supplement on insulin sensitivity, glucose effectiveness, and acute insulin response after glucose load in male type 2 diabetics. Endocrine Res 2005;31:139—148.
- Cohen JC, Hickman R. Insulin resistance and diminished glucose tolerance in powerlifters ingesting anabolic steroids. J Clin Endocrinol Metab 1987;64:960—3.
- Aldercreutz H, Mazur W. Phyto-estrogens and western diseases. Annals of Medicine 1997;29:95—120.
- Ranexa (ranolazine extended-release tablets) package insert. Foster City, CA: Gilead Sciences, Inc. 2013 Dec.
- Letairis™ (ambrisentan) package insert. Foster City, CA: Gilead Sciences, Inc; 2008 Oct.
- Pradaxa (dabigatran) package insert. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc.; 2015 Jan.
- Gilotrif (afatinib) package insert. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2013 Nov.
- Androgel 1.62% (testosterone gel) package insert. North Chicago, IL: Abbott Laboratories; 2014 Nov.
- Naik BS, Shetty N, Maben EVS. Drug-induced taste disorders. European Journal of Internal Medicine 2010; 21:240-243.”
Related medications
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
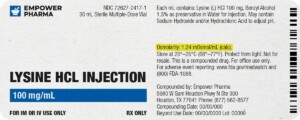
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.






 DHEA Cream
DHEA Cream Tadalafil / Oxytocin ODT
Tadalafil / Oxytocin ODT Metformin Tablets
Metformin Tablets Pseudoephedrine Tablets
Pseudoephedrine Tablets Estradiol Capsules
Estradiol Capsules Zomacton Injection
Zomacton Injection Nandrolone Decanoate / Testosterone Cypionate / Testosterone Enanthate Injection
Nandrolone Decanoate / Testosterone Cypionate / Testosterone Enanthate Injection Tadalafil / Phentolamine Mesylate Capsules
Tadalafil / Phentolamine Mesylate Capsules Bi-Est Vaginal Cream
Bi-Est Vaginal Cream Progesterone Gel (Crinone®)
Progesterone Gel (Crinone®)