Rosacea INO Gel
This product is available solely through our 503A Compounding Pharmacy, ensuring personalized care and precision in every order. Please note that a valid prescription is required for purchase. If you do not have an account, please contact us.
Product Overview
Ivermectin
Ivermectin (dihydroavermectin B1) is an antiparasitic agent of the avermectin class. Ivermectin has structural similarities to the macrolide antibiotics but lacks antibacterial activity. Avermectins are produced naturally by the actinomycete Streptomycetes avermetilis. Ivermectin lotion is used topically to treat Pediculosis capitis (head lice). Ivermectin cream is used topically for the treatment of inflammatory lesions of rosacea. Oral ivermectin is used in treating infections due to Onchocerca volvulus (onchocerciasis) or Strongyloides stercoralis(strongyloidiasis). Ivermectin is only active against the tissue microfilariae of Onchocerca volvulus and the intestinal stage of Strongyloides stercoralis; ivermectin has no activity against adult Onchocerca volvulus. Although not FDA-approved for infections due to Sarcoptes scabiei (scabies), crusted (Norwegian) scabies, or superinfected scabies, ivermectin has been used successfully to treat these conditions.[1][2] Ivermectin is effective against the circulating microfilariae of Wuchereria bancrofti (responsible for Bancroft’s filariasis) and other major filarial diseases (i.e., Loa loa).[3] However, ivermectin is not effective against Mansonella perstans.[4] Ivermectin has also demonstrated promise for the treatment of nematodes such as cutaneous larva currens and localized and disseminated cutaneous larva migrans. Ivermectin is recommend by The World Health Organization (WHO) for treating onchocerciasis (river blindness) and lymphatic filariasis (Bancroft’s filariasis). Resistance to ivermectin has not been reported. Ivermectin oral tablets were FDA-approved in November 1996.
Niacinamide
Niacin (nicotinic acid or 3-pyridinecarboxylic acid) is a B-complex vitamin. Good dietary sources of niacin are animal proteins, beans, green vegetables, liver, mushrooms, peanuts, whole wheat, and unpolished rice. Niacin is also present in cereal grains but is largely bound to plant proteins, and thus is poorly absorbed after ingestion. Niacin is one of the substances used in the enrichment of refined flour, and our dietary intake of pre-formed niacin comes primarily from enriched grains. However, the body’s niacin requirement is also met by the biosynthesis of niacin from tryptophan, an amino acid. For example, milk and eggs do not contain niacin, but do contain large amounts of tryptophan from which niacin is derived. Each 60 mg of excess tryptophan (after protein synthesis) is converted to approximately 1 mg of niacin. Synthesis of the vitamin from tryptophan in proteins supplies roughly half the niacin requirement in man. Iron-deficiency or inadequate pyridoxine or riboflavin status will decrease the conversion of tryptophan to niacin and may contribute to deficiency, due to an interdependence of coenzymes in the niacin production pathway. A late and serious manifestation of niacin deficiency is pellagra, a clinical symptom complex principally affecting the GI tract, skin, and CNS, producing symptoms of diarrhea, dermatitis, and dementia, respectively. Pellagra may result from a niacin- and protein-deficient diet, isoniazid therapy, or certain diseases that result in poor utilization of tryptophan. Pellagra was the only vitamin-deficiency disease to ever reach epidemic proportions in the US; pellagra is rare today in industrialized countries due to the enrichment of refined flours.
Several synonyms for niacin and niacinamide exist. Synthetic niacin could be produced by the oxidation of nicotine, and the term ‘nicotinic acid’ evolved. Scientists also coined the terms ‘nicotinamide’ and ‘niacinamide’ for the amide form of nicotinic acid. The term ‘niacin’ has been used generically since the 1940’s to label foods and to avoid association of the vitamins with the nicotine alkaloid from tobacco. Thus, the name ‘niacin’ has been used to denote both chemical forms, which are equivalent as vitamins on a weight basis. Both nicotinic acid and nicotinamide are synthesized for inclusion in nutritional supplements. However, since nicotinic acid and nicotinamide have different pharmacologic properties outside of their use as vitamins, it is important to distinguish between the two forms in pharmaceutical products.
In clinical medicine, nicotinic acid is used as an antilipemic, but nicotinamide (niacinamide) is not effective for this purpose. Nicotinic acid was the first hypolipidemic agent shown to decrease the incidence of secondary myocardial infarction (MI) and reduce total mortality in MI patients. However, no incremental benefit of coadministration of extended-release niacin with lovastatin or simvastatin on cardiovascular morbidity and mortality over and above that demonstrated for extended-release niacin, simvastatin, or lovastatin monotherapy has been established. In addition, the AIM-HIGH trial demonstrated that the concurrent use of extended-release niacin (1500—2000 mg/day PO) and simvastatin does not result in a greater reduction in the incidence of cardiovascular events than simvastatin alone.[5] These results are consistent with those of the larger HPS2-THRIVE trial in which the addition of extended-release niacin to effective statin-based therapy did not result in a greater reduction in the incidence of cardiovascular events. Furthermore, there was an increased risk of serious adverse events including an increased incidence of disturbances in diabetes control and diabetes diagnoses, as well as serious gastrointestinal, musculoskeletal, dermatological, infectious, and bleeding adverse events. There was also a statistically insignificant 9% proportional increase in the incidence of death from any cause in the niacin group.[6] The ARBITER 6-HALTS trial demonstrated that the addition of extended-release niacin 2000 mg/day to statins results in significant regression in atherosclerosis as measured by carotid intima-media thickness, and is superior to the combination of ezetimibe and a statin.[7] In an MRI study, the addition of extended-release niacin 2000 mg/day to statin therapy resulted in a significant reduction in carotid wall area compared to placebo.[8] However, the NIA Plaque study, which was presented at the American Heart Association (AHA) 2009 Scientific Sessions, did not find a significant reduction in the progression of atherosclerosis associated with the addition of niacin to statin therapy as compared to statin monotherapy. Additionally, nicotinic acid has been used as a therapy for tinnitus, but efficacy data are scant. Some sustained-release nicotinic acid formulations have a lower incidence of flushing but a higher incidence of hepatotoxicity when compared to immediate-release forms.[9] Some dosage forms are available without prescription. The FDA officially approved niacin in 1938.
Oxymetazoline Hydrochloride
Oxymetazoline is an alpha adrenoreceptor agonist that acts as a topically applied sympathomimetic vasoconstrictor. Oxymetazoline is available as a topical cream, ophthalmic solution, and an intranasal spray. The topical cream is approved to treat persistent facial erythema in adults with rosacea. Oxymetazoline administered as an ophthalmic preparation relieves redness of the eye due to minor eye irritants. The intranasal formulation is indicated to treat nasal congestion associated with acute or chronic rhinitis, sinusitis, the common cold, hay fever, and other allergies. The maximum recommended treatment duration for the intranasal spray is 3 days; excessive or prolonged use can cause nasal mucosa irritation and recurrent nasal congestion. This drug was approved by the FDA in 1964.[10][11][12]
Ivermectin
Avermectins, including ivermectin, are broad-spectrum antiparasitic agents. They bind selectively and with high affinity to glutamate-gated chloride ion channels present in invertebrate nerve and muscle cells. This binding leads to an increase in the permeability of the cell membrane to chloride ions with hyperpolarization of the nerve or muscle cell, resulting in paralysis and death of the parasite. This class of compounds may also bind with other ligand-gated chloride channels, such as those gated by the neurotransmitter gamma-aminobutyric acid (GABA). The avermectins’ selectivity is due to the fact that some mammals do not have glutamate-gated chloride channels and that the avermectins have a low affinity for mammalian ligand-gated chloride channels. Ivermectin does not cross the blood-brain barrier in humans.
Niacinamide
Dietary requirements for niacin can be met by the ingestion of either nicotinic acid or nicotinamide; as vitamins, both have identical biochemical functions. As pharmacologic agents, however, they differ markedly. Nicotinic acid is not directly converted into nicotinamide by the body; nicotinamide is only formed as a result of coenzyme metabolism. Nicotinic acid is incorporated into a coenzyme known as nicotinamide adenine dinucleotide (NAD) in erythrocytes and other tissues. A second coenzyme, nicotinamide adenine dinucleotide phosphate (NADP), is synthesized from NAD. These two coenzymes function in at least 200 different redox reactions in cellular metabolic pathways. Nicotinamide is released from NAD by hydrolysis in the liver and intestines and is transported to other tissues; these tissues use nicotinamide to produce more NAD as needed. Together with riboflavin and other micronutrients, the NAD and NADP coenzymes work to convert fats and proteins to glucose and assist in the oxidation of glucose.
In addition to its role as a vitamin, niacin (nicotinic acid) has other dose-related pharmacologic properties. Nicotinic acid, when used for therapeutic purposes, acts on the peripheral circulation, producing dilation of cutaneous blood vessels and increasing blood flow, mainly in the face, neck, and chest. This action produces the characteristic “niacin-flush”. Nicotinic acid-induced vasodilation may be related to release of histamine and/or prostacyclin. Histamine secretion can increase gastric motility and acid secretion. Flushing may result in concurrent pruritus, headaches, or pain. The flushing effects of nicotinic acid appear to be related to the 3-carboxyl radical on its pyridine ring. Nicotinamide (niacinamide), in contrast to nicotinic acid, does not contain a carboxyl radical in the 3 position on the pyridine ring and does not appear to produce flushing.
Nicotinic acid may be used as an antilipemic agent, but nicotinamide does not exhibit hypolipidemic activity. Niacin reduces total serum cholesterol, LDL, VLDL, and triglycerides, and increases HDL cholesterol. The mechanism of nicotinic acid’s antilipemic effect is unknown but is unrelated to its biochemical role as a vitamin. One of nicotinic acid’s primary actions is decreased hepatic synthesis of VLDL. Several mechanisms have been proposed, including inhibition of free fatty acid release from adipose tissue, increased lipoprotein lipase activity, decreased triglyceride synthesis, decreased VLDL-triglyceride transport, and an inhibition of lipolysis. This last mechanism may be due to niacin’s inhibitory action on lipolytic hormones. Nicotinic acid possibly reduces LDL secondary to decreased VLDL production or enhanced hepatic clearance of LDL precursors. Nicotinic acid elevates total HDL by an unknown mechanism, but is associated with an increase in serum levels of Apo A-I and lipoprotein A-I, and a decrease in serum levels of Apo-B. Nicotinic acid is effective at elevating HDL even in patients whose only lipid abnormality is a low-HDL value. Niacin does not appear to affect the fecal excretion of fats, sterols, or bile acids. Clinical trial data suggest that women have a greater hypolipidemic response to niacin therapy than men at equivalent doses.
Oxymetazoline Hydrochloride
Oxymetazoline stimulates alpha adrenergic receptors which cause intense vasoconstriction. When administered intranasally, this action promotes drainage and improves ventilation. Ophthalmic administration causes vasoconstriction of conjunctival blood vessels thereby providing relief from minor eye irritations. In patients with rosacea, topical use can reduce facial erythema.[10][11][12]
Ivermectin
Ivermectin is contraindicated in patients with hypersensitivity to any component of the product.[13]
Patients with a history of severe asthma should receive ivermectin with caution. Occasionally, systemic ivermectin has been reported to worsen bronchial asthma.[13]
Although not extensively studied, due to its extensive hepatic metabolism, ivermectin should be administered with caution in patients with significant hepatic disease.[13]
In patients with immunosuppression (including those with human immunodeficiency virus (HIV) infection) treated for intestinal strongyloidiasis, repeated ivermectin courses may be necessary. Adequate and well-controlled clinical studies have not been conducted in such patients to determine the optimal dosing regimen. Several treatments (i.e., at 2 week intervals) may be required and a cure may not be achievable. Control of extra-intestinal strongyloidiasis in these patients is difficult, however, suppressive therapy (i.e., once per month) may be helpful.[13]
Data with oral ivermectin use during pregnancy are insufficient to inform a drug-associated risk. Systemic exposure from topical use of ivermectin is much lower than from oral use. Four published epidemiology studies evaluated the outcomes of a total of 744 women exposed to oral ivermectin in various stages of pregnancy. In the largest study, 397 women in the second trimester of pregnancy were treated open-label with single doses of ivermectin or ivermectin plus albendazole; there was no observed difference in pregnancy outcomes between treated and untreated populations. However, these studies cannot definitely establish or exclude the absence of drug-associated risk during pregnancy, because either the timing of the administration during gestation was not accurately ascertained or the administration only occurred during the second trimester. In animal embyrofetal development studies of oral ivermectin given during organogenesis, adverse developmental outcomes, including cleft palate, exencephaly, wavy ribs, and clubbed forepaws, occurred at or near doses that were maternally toxic. Pre-implantation loss and abortion were also noted.[14][13][15]
After oral administration, ivermectin is excreted in human breast milk in low concentrations. There is insufficient evidence to determine its effects on the breast-fed infant or milk production.[13][14]It is estimated that an exclusively breast-fed infant would receive less than 1% of the maternal weight adjusted maternal dose.[16] According to the manufacturer, treatment with oral ivermectin in mothers who are breast-feeding should only be undertaken when the risk of delayed treatment to the mother outweighs the possible risk to the newborn.[13] Previous American Academy of Pediatrics (AAP) recommendations considered oral ivermectin to be usually compatible with breast-feeding.[17] The amount of ivermectin present in human milk after topical application has not been studied; however, systemic exposure from topical ivermectin use is much lower than from oral use. According to the manufacturer, discontinue nursing or discontinue the topical cream, taking into account the importance of the drug to the mother. Consider the developmental and health benefits of breast-feeding along with the mother’s clinical need for the topical lotion and any potential adverse effects on the breast-fed infant from the topical lotion or the underlying maternal condition. Women who are breast-feeding while using topical ivermectin should avoid accidental transfer of ivermectin to the breast area where it might be directly ingested while nursing.[14][15]
Ivermectin oral tablets are approved for use in children >= 15 kg of weight. Safe and effective use has not been established in neonates, infants or children weighing less than 15 kg. The topical administration of ivermectin to children should be under the direct supervision of an adult to prevent ingestion of the lotion and/or cream. The safety and efficacy of ivermectin lotion have not been established in neonates or infants < 6 months. Topical ivermectin lotion is not recommended in pediatric patients < 6 months because of the potential for increased systemic absorption due to a ratio of skin surface area to body mass. There is also a potential increased risk of ivermectin toxicity due to an immature skin barrier. The safety and efficacy of ivermectin cream have not been established in children < 18 years of age.[13][14][15] Rarely, patients with onchocerciasis and Loa loa coinfection may develop a serious or even fatal encephalopathy either spontaneously or after treatment with an effective microfilaricide. This syndrome has been seen very rarely after the use of ivermectin. In individuals who warrant treatment with ivermectin for any reason and have had significant exposure to Loa loa-endemic areas of West and Central Africa, pretreatment assessment for loiasis and careful posttreatment follow-up is recommended.[13] Patients with hyperreactive onchodermatitis (i.e., sowda) may be more likely than others to experience severe edema and worsening of onchodermatitis after ivermectin use.[13]
Niacinamide
Patients who have a known hypersensitivity to niacin or any product component should not be given the drug.
While steady state plasma concentrations of niacin are generally higher in women than in men, the absorption, metabolism, and excretion of niacin appears to be similar in both genders. Women have been reported to have greater response to the lipid-lowering effects of nicotinic acid (niacin) when compared to men.
No overall differences in safety and efficacy were observed between geriatric and younger individuals receiving niacin. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity for some older individuals cannot be ruled out.
Niacin is contraindicated in patients who have significant or unexplained hepatic disease. Patients who consume large quantities of ethanol (alcoholism), who have risk factors for hepatic disease, or who have a past-history of gallbladder disease, jaundice, or hepatic dysfunction may receive niacin with close clinical observation. Elevations in liver function tests (LFTs) appear to be dose-related. Some sustained-release nicotinic acid (niacin) formulations have a higher incidence of hepatotoxicity when compared to immediate-release dosage forms. Extended-release nicotinic acid preparations (e.g., Niaspan, Slo-Niacin) should not be substituted for equivalent dosages of immediate-release (crystalline) niacin (e.g., Niacor and others). Follow the manufacturer-recommended initial dosage titration schedules for extended-release products, regardless of previous therapy with other niacin formulations. Monitor LFTs in all patients during therapy at roughly 6-month intervals or when clinically indicated. If transaminase levels (i.e., ALT or AST) rise to 3 times the upper limit of normal, or clinical symptoms of hepatic dysfunction are present, niacin should be discontinued.
Nicotinic acid (niacin) can stimulate histamine release, which, in turn, can stimulate gastric acid output. Niacin is contraindicated in patients with active peptic ulcer disease (PUD) because it can exacerbate PUD symptoms. Use niacin with caution in patients with a past history of peptic ulcer disease or in those on maintenance therapy to prevent PUD recurrence.
Due to its vasodilatory action, nicotinic acid (niacin) should be used with caution in those patients with uncorrected hypotension (or predisposition to orthostatic hypotension), acute myocardial infarction, or unstable angina, particularly when vasodilator medications such as nitrates, calcium channel blockers, or adrenergic blocking agents are coadministered (see Drug Interactions). Because the vasodilatory response to niacin may be more dramatic at the initiation of treatment, activities requiring mental alertness (e.g., driving or operating machinery) should not be undertaken until the response to niacin is known.
Niacin, especially in high doses, can cause hyperuricemia. Niacin should be prescribed cautiously to patients with gout (or predisposed to gout). These individuals should be advised not to purchase OTC forms of niacin without the guidance of a physician.
Niacin, especially in high doses, can cause hypophosphatemia. Although the reductions in phosphorus levels are usually transient, clinicians should monitor serum phosphorus periodically in those at risk for this electrolyte imbalance.
Rare cases of rhabdomyolysis have been reported in patients taking lipid-altering dosages of nicotinic acid (niacin) and statin-type agents concurrently (see Drug Interactions). Patients undergoing combined therapy should be carefully monitored for muscle pain, tenderness, or weakness, particularly in the early months of treatment or during periods of upward dose titration of either drug. While periodic CPK and potassium determinations may be considered, there is no evidence that these tests will prevent the occurrence of severe myopathy. If rhabdomyolysis occurs, the offending therapies should be discontinued.
Niacin, especially in high doses, may cause hyperglycemia. Niacin should be prescribed cautiously to patients with diabetes mellitus. These individuals should be advised not to purchase OTC forms of niacin without the guidance of a physician. Niacin has also been reported to cause false-positive results in urine glucose tests that contain cupric sulfate solution (e.g., Benedict’s reagent, Clinitest).
Niacin therapy has been used safely in children for the treatment of nutritional niacin deficiency. However, the safety and effectiveness of nicotinic acid for the treatment of dyslipidemias have not been established in neonates, infants and children <= 16 years of age. Nicotinic acid has been used for the treatment of dyslipidemia in pediatric patients under select circumstances. Children may have an increased risk of niacin-induced side effects versus adult populations. At least one pediatric study has concluded that niacin treatment should be reserved for treatment of severe hypercholesterolemia under the close-supervision of a lipid specialist.[18] In general, the National Cholesterol Education Program (NCEP) does not recommend drug therapy for the treatment of children with dyslipidemias until the age of 10 years or older.[19] Since niacin is an essential nutrient, one would expect it to be safe when administered during pregnancy at doses meeting the recommended daily allowance (RDA). Niacin is categorized as pregnancy category A under these conditions. However, when used in doses greater than the RDA for dyslipidemia, or when used parenterally for the treatment of pellagra, niacin is categorized as pregnancy category C. Most manufacturers recommend against the use of niacin in dosages greater than the RDA during pregnancy. The potential benefits of high-dose niacin therapy should be weighed against risks, since toxicological studies have not been performed.[5] According to a manufacturer of niacin (Niaspan), although no studies have been conducted in nursing mothers, excretion into human milk is expected. The manufacturer recommends the discontinuation of nursing or the drug due to serious adverse reactions that may occur in nursing infants from lipid-altering doses of nicotinic acid.[5] Niacin, in the form of niacinamide, is excreted in breast milk in proportion to maternal intake. Niacin supplementation is only needed in those lactating women who do not have adequate dietary intake. The Recommended Daily Allowance (RDA) of the National Academy of Science for niacin during lactation is 20 mg.[20] There are no safety data regarding the use of nicotinic acid in doses above the RDA during breast-feeding. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA. Use niacin with caution in patients with renal disease (renal failure or severe renal impairment) since niacin metabolites are excreted through the kidneys. It appears that no special precautions are needed when administering niacin to meet the recommended nutritional daily allowance (RDA). Use caution when administering higher dosages. Nicotinic acid (niacin) occasionally causes slight decreases in platelet counts or increased prothrombin times and should be used with caution in patients with thrombocytopenia, coagulopathy, or who are receiving anticoagulant therapy. Patients who will be undergoing surgery should have blood counts monitored. Nicotinic acid (niacin) is contraindicated in patients with arterial bleeding. The federal Omnibus Budget Reconciliation Act (OBRA) regulates medication use in residents (e.g., geriatric adults) of long-term care facilities (LTCFs). According to OBRA, glucose and liver function tests should be evaluated regularly because niacin interferes with glucose control, can aggravate diabetes, and can exacerbate active gallbladder disease and gout. Flushing is a common side effect of niacin.[21]
Oxymetazoline Hydrochloride
Take care to avoid ocular exposure during use of oxymetazoline topical cream and nasal spray formulations. To avoid accidental exposure of non-treatment sites, instruct patients to wash hands immediately after applying the topical cream. Prior to use of the ophthalmic solution, contact lenses must be removed.[10][11][12]
Caution is advised when administering oxymetazoline to patients receiving concurrent MAOI therapy. Monoamine oxidase inhibitors can affect the metabolism and uptake of circulating amines; thereby potentiating the vasoconstrictive effects of oxymetazoline.[10]
Oxymetazoline (an alpha-adrenergic agonist) acts as a vasoconstrictor, which may adversely affect blood pressure; thus, caution is advised when administering the drug to patients with severe or unstable cardiovascular diseases, orthostatic hypotension, and uncontrolled hypertension or hypotension. Instruct patients with cardiac disease to seek immediate medical attention if their condition worsens.[10][11]
Caution is advised when administering oxymetazoline (a vasoconstrictor) to patients with vascular and autoimmune diseases, such as coronary artery disease, cerebrovascular disease, diabetes mellitus, thyroid disease, prostatic hypertrophy, Sjogren’s syndrome, Raynaud’s phenomenon, thromboangiitis obliterans (Buerger’s disease), and scleroderma. Instruct patients to seek immediate medical care if signs or symptoms of worsening vascular insufficiency develops.[10][11]
Treatment with oxymetazoline may increase the risk of developing angle closure glaucoma in patients with closed-angle glaucoma. Instruct patients to seek immediate medical care if signs or symptoms of acute angle closure glaucoma develop.[10][12]
Safety and efficacy of oxymetazoline topical cream have not been established in pediatric patients younger than 18 years of age (i.e., neonates, infants, children, and adolescents); however, the ophthalmic solution and nasal spray may be used in children as young as 6 years of age.[10][11][12]
Data are limited regarding use of oxymetazoline during pregnancy. No adequate and well-controlled trials have been conducted, and it is unknown if the drug causes fetal harm or adverse pregnancy outcomes. Data from one literature article found a potential association between second trimester exposure to oxymetazoline nasal spray and renal collecting system anomalies. In another case, fetal distress was reported in a 41-week pregnant patient following repeated use of oxymetazoline nasal spray at a dose 5-times the recommended dose. The fetal distress resolved hours later, and prior to delivery of the healthy infant. Exposure to oxymetazoline topical cream has also been reported in two pregnant females. One pregnancy resulted in delivery of a healthy child. The other pregnancy ended in spontaneous abortion, which was not considered related to drug exposure.[10]
It is not known whether oxymetazoline is distributed into breast milk, or if the drug affects breast milk production. According to the manufacturer, caution should be exercised when administering it to women who are breast-feeding their infants. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA.[10]
Ivermectin
Ivermectin is generally well tolerated, particularly with single-dose use. Compared to other antiparasitics used for similar indications, fewer adverse effects and better compliance are usually seen with ivermectin. Adverse events are typically not dose-related. The side effects reported in clinical experience have varied according to the underlying disease or indication for treatment. In patients being treated for onchocerciasis, the most common adverse reactions were related to allergic and inflammatory responses to the death of the microfilariae (the Mazzotti reaction). Especially in severe onchocerciasis disease, ivermectin may be administered with a corticosteroid, an antihistamine, or another antiinflammatory agent to minimize these reactions. Patients with hyperreactive onchodermatitis (sowda) may be more likely than others to experience severe adverse reactions, especially edema and aggravation of onchodermatitis. Mazzotti-type and ophthalmologic reactions associated with the treatment of onchocerciasis or the disease itself would not be expected in patients with strongyloidiasis being treated with ivermectin.[13]
In patients being treated for onchocerciasis with ivermectin, adverse reactions related to allergic and inflammatory responses to the death of the microfilariae (the Mazzotti reaction) include arthralgia/synovitis (9.3%) as well as axillary, cervical, inguinal, and other lymph node enlargement (lymphadenopathy, 3—12.6%) and tenderness (1.2—13.9%).[13]
In patients being treated for onchocerciasis with systemic ivermectin, adverse reactions related to allergic and inflammatory responses to the death of the microfilariae (the Mazzotti reaction) include pruritus (27.5%) and other skin involvement that may manifest as angioedema (1.2%), peripheral edema (3.2%), rashes including maculopapular rash, pustular rash, or urticaria (22.7%). Adverse reactions associated with strongyloidiasis treatment include pruritus (2.8%), rash (unspecified) (0.9%), and urticaria (0.9%). Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported with ivermectin use in postmarketing experience.[13] Adverse reactions reported in 1% or less of patients treated with ivermectin topical lotion and/or cream in trials include xerosis, and skin burning sensation/skin irritation.[14][15] Contact dermatitis and allergic dermatitis were reported in postmarketing use of ivermectin topical cream.[15]
In patients being treated for onchocerciasis with ivermectin, adverse reactions related to allergic and inflammatory responses to the death of the microfilariae (the Mazzotti reaction) include fever (22.6%).[13]
Adverse reactions associated with ivermectin used for strongyloidiasis treatment include asthenia/fatigue (0.9%).[13]
Adverse reactions associated with ivermectin used for strongyloidiasis treatment include abdominal pain (0.9%), anorexia (0.9%), constipation (0.9%), diarrhea(1.8%), and nausea (1.8%), vomiting (0.9%).[13]
Adverse reactions associated with ivermectin used for strongyloidiasis treatment include dizziness (2.8%), somnolence/drowsiness (0.9%), vertigo (0.9%), and tremor (0.9%). Seizures have been reported with ivermectin use in post-marketing experience.[13]
Ophthalmological conditions (i.e., limbitis, punctate opacity) were examined in clinical trials in 963 adult onchocerciasis patients who received 100—200 mcg/kg of ivermectin. The ophthalmological changes observed were primarily deterioration from baseline 3 days post-treatment. Most changes returned to baseline or improved over baseline after 3—6 months. Significant adverse effects, such as visual impairment (e.g., loss of vision), do rarely occur and can occur with river blindness itself, but have also been reported with ivermectin therapy. These effects include abnormal sensation of the eyes, eyelid edema, anterior uveitis, conjunctivitis, limbitis, keratitis, and chorioretinitis or choroiditis. These effects generally resolve after treatment with corticosteroids. Conjunctival hemorrhage (ocular hemorrhage) has been reported with systemic ivermectin use for onchocerciasis in post-marketing experience.[13] Adverse reactions reported in < 1% of subjects treated with ivermectin lotion in placebo-controlled trials include conjunctivitis, ocular hyperemia, and ocular irritation.[14] Orthostatic hypotension (1.1%) and sinus tachycardia (3.5%) have been reported with systemic ivermectin use.[13] Elevated hepatic enzymes have been reported in 2% of patients treated with systemic ivermectin. Hepatitis and hyperbilirubinemia have been reported post-marketing.[13] Rarely, patients with onchocerciasis who are also heavily infected with Loa loa may develop a serious or even fatal encephalopathy, either spontaneously or after treatment with an effective microfilaricide. This syndrome has been seen very rarely after the use of ivermectin. These patients may also experience back pain, neck pain, red eye, conjunctival hemorrhage, dyspnea, urinary incontinence, fecal incontinence, difficulty in standing/walking, mental status changes, confusion, lethargy, stupor, seizures, or coma.[13] Although studies are conflicted, patients treated with ivermectin may have prolonged bleeding time due to a potential antagonistic effect with vitamin K. One study reported hematomatous swellings in 2 of 28 onchocerciasis patients treated with ivermectin, with prothrombin times significantly above baseline from one week to one month after treatment.[22] An additional study showed prolonged prothrombin ratios in 148 patients given ivermectin. There were no reported bleeding complications; however, Factor II and VII levels were reduced in most patients with increased prothrombin times.[23] In contrast, another study of 20 patients reported no changes in prothrombin times compared with baseline for 13 days after treatment.[24] Bleeding disorders were also not found in 15,000 patients treated with ivermectin.[25] Although there is no direct interaction with warfarin noted in the literature, coadministration of ivermectin and warfarin should be used with caution as there may be potentiation of prolonged prothrombin time. Post-marketing reports of increased INR have been rarely reported with the co-administration of ivermectin and warfarin.[13] Patients with potential increased prothrombin times, such as those on warfarin, should use ivermectin with caution. Decreased leukocyte count (3%), eosinophilia (3%), and increased hemoglobin (1%) have been reported with the use of systemic ivermectin. Leukopenia and and anemia were reported in one patients treated for strongyloidiasis.[13]
Niacinamide
Niacin (nicotinic acid), when administered in doses equivalent to the RDA, is generally nontoxic. Niacinamide also rarely causes adverse reactions. Larger doses of nicotinic acid (i.e., >= 1 g/day PO), can cause adverse reactions more frequently. Differences in adverse reaction profiles can be explained by the fact that nicotinic acid has pharmacologic properties that are different from niacinamide.
Peripheral vasodilation is a well-known adverse reaction to niacin. It is characterized by flushing; warmth; and burning or tingling of the skin, especially in the face, neck, and chest. Hypotension can be caused by this vasodilation. Patients should avoid sudden changes in posture to prevent symptomatic or orthostatic hypotension. Dizziness and/or headache, including migraine, can occur. Cutaneous flushing is more likely to occur with immediate-release preparations as opposed to sustained-release ones and also increases in incidence with higher doses.[9] Following 4-weeks of maintenance therapy of 1500 mg daily, patients receiving immediate release niacin averaged 8.6 flushing events compared to 1.9 events in the Niaspan group. In placebo-controlled studies of Niaspan, flushing occurred in 55—69% of patients compared to 19% of patients receiving placebo. Flushing was described as the reason for discontinuing therapy for 6% of patients receiving Niaspan in pivotal studies.[5] These reactions usually improve after the initial 2 weeks of therapy. Some patients develop generalized pruritus as a result of peripheral flushing. In placebo controlled trials, pruritus was reported in 0—8% of patients receiving Niaspan compared to 2% of patients taking placebo. Rash (unspecified) was reported in 0—5% of patients in the Niaspan group compared to no patients in the placebo group.[5] Patients should avoid ethanol or hot drinks that can precipitate flushing. Flushing can be minimized by taking niacin with meals, using low initial doses, and increasing doses gradually. If necessary, taking one aspirin (e.g., 325 mg) 30 minutes before each dose can help prevent or reduce flushing. Spontaneous reports with niacin suggest that flushing may also be accompanied by symptoms of dizziness or syncope, sinus tachycardia, palpitations, atrial fibrillation, dyspnea, diaphoresis, chills, edema, or exacerbations of angina. On rare occasions, cardiac arrhythmias or syncope has occurred. Hypersensitivity or anaphylactoid reactions have been reported rarely during niacin therapy; episodes have included one or more of the following features: anaphylaxis, angioedema, urticaria, flushing, dyspnea, tongue edema, laryngeal edema, face edema, peripheral edema, laryngospasm, maculopapular rash, and vesiculobullous rash (vesicular rash, bullous rash).
Niacin can produce a variety of GI effects, such as nausea/vomiting, abdominal pain, diarrhea, bloating, dyspepsia, or flatulence, when taken in large doses. Eructation and peptic ulcer has been reported with post-marketing experience of Niaspan. Compared to placebo, diarrhea was reported in 7—14% (vs. 13%), nausea in 4—11% (vs. 7%), and vomiting in 0—9% (vs. 4%) of patients receiving Niaspan.[5] These effects are attributed to increased GI motility and may disappear after the first 2 weeks of therapy. Administering niacin with meals can reduce these adverse reactions.
Jaundice can result from chronic liver damage caused by niacin. It has been shown that elevated hepatic enzymes occur more frequently with some sustained-release niacin than with immediate-release products.[9] However, in a study of 245 patients receiving Niaspan (doses ranging from 500—3000 mg/day for a mean of 17 weeks) no patients with normal serum transaminases at baseline experienced elevations to > 3x the upper limit of normal. Sustained-release products have been associated with post-marketing reports of hepatitis and jaundice, including Niaspan. Regular liver-function tests should be performed periodically. The changes in liver function induced by niacin are typically reversible with drug discontinuation. However, rare cases of fulminant hepatic necrosis and hepatic failure have been reported. Some cases have occurred after the substitution of sustained-release dosage forms for immediate-release products at directly equivalent doses; these dosage forms are not bioequivalent. Dosage titration schedules must be observed for any patient switched to a sustained-release niacin product, even if the patient was previously taking immediate-release therapy.[5]
Niacin interferes with glucose metabolism and can result in hyperglycemia.[5] This effect is dose-related. During clinical anti-lipemic trials, increases in fasting blood glucose above normal occurred frequently (e.g., 50%) during niacin therapy. Some patients have required drug discontinuation due to hyperglycemia or exacerbation of diabetes. In the AIM-HIGH trial of patients with stable cardiovascular disease, the incidence of hyperglycemia (6.4% vs. 4.5%) and diabetes mellitus (3.6% vs. 2.2%) was higher in niacin plus simvastatin-treated patients compared to the simvastatin plus placebo group. Close blood glucose monitoring is advised for diabetic or potentially diabetic patients during treatment with niacin; adjustment of diet and/or antidiabetic therapy may be necessary.[5]
Niacin, especially in high doses, can cause hyperuricemia. Gout has been reported in post-marketing surveillance of Niaspan.[5] Therefore, patients predisposed to gout should be treated with caution.
Niacin, especially in high doses (>= 2 g/day PO), can cause hypophosphatemia (mean decrease 13%). Serum phosphorus concentrations should be monitored periodically in patients at risk for hypophosphatemia.[5]
Nicotinic acid (niacin) occasionally causes slight decreases in platelet counts (mean reduction 11%) or increased prothrombin times (mean increase 4%), especially in high doses (>= 2 g/day PO). Rarely do these reactions result in coagulopathy or thrombocytopenia, but clinically significant effects might occur in patients with other risk factors or who are predisposed to these conditions.[5]
Asthenia, nervousness, insomnia, and paresthesias have been reported during niacin therapy. Rare cases of rhabdomyolysis have been reported in patients taking niacin (nicotinic acid) in doses >=1 g/day PO and HMG-CoA reductase inhibitors (i.e., ‘statins’) concurrently. In the AIM-HIGH trial, 4 cases (0.2%) of rhabdomyolysis were reported in the niacin; simvastatin group compared with 1 case in the simvastatin plus placebo group. Rhabdomyolysis may present as myopathy (myalgia, myasthenia, muscle cramps, muscle weakness, muscle tenderness, fatigue), elevations in creatinine phosphokinase (CPK), or renal dysfunction (renal tubular obstruction). Toxicity to the skeletal muscle occurs infrequently but can be a serious adverse reaction. This toxicity appears to be reversible after discontinuation of therapy.[5]
Niacin also has been associated with a variety of ophthalmic adverse effects including blurred vision and macular edema.[5]
Although uncommon, niacin may be associated with skin hyperpigmentation or acanthosis nigricans. Dry skin (xerosis) also has been reported during post-marketing surveillance of Niaspan.[5][26]
During clinical trials, increased cough was reported in <2—8% (vs. 6%) of patients receiving Niaspan compared to placebo.[5]
Oxymetazoline Hydrochloride
Serious and life-threatening adverse events requiring hospitalization have been reported to the FDA after children 5 years of age and younger accidentally ingested over-the-counter (OTC) oxymetazoline ophthalmic drops and nasal sprays. No deaths were reported; however, events such as nausea, vomiting, lethargy, sinus tachycardia, respiratory depression, bradycardia, hypotension, hypertension, sedation, somnolence, mydriasis, stupor, hypothermia, drooling, and coma have occurred. Serious adverse events can occur following ingestion of only a small amount (1 to 2 mL) in young children. Since most of these OTC products do not contain child-resistant closures, it is imperative that patients store these products out of reach of children. If a child accidentally swallows these drops, call the National Capital Poison Center (1-800-222-1222) and seek emergency medical attention immediately.[27]
During clinical trials, oxymetazoline topical cream was associated with application site reactions, including contact dermatitis (2% to 3%), pruritus (1% to 2%), erythema (1% to 2%), and pain (1% to 2%). In addition, 1% to 3% of drug recipients experienced worsening inflammatory lesions of rosacea.[10]
The maximum recommended treatment duration for oxymetazoline nasal spray is 3 days. Prolonged use may result in recurrent or worsening nasal congestion. Other adverse events associated with use of the nasal spray include nasal irritation (i.e., burning or stinging), rhinorrhea, and sneezing.[11]
Ocular irritation, ocular pain, and visual impairment may occur during use of oxymetazoline ophthalmic solution.[12]
Ivermectin
Data with oral ivermectin use during pregnancy are insufficient to inform a drug-associated risk. Systemic exposure from topical use of ivermectin is much lower than from oral use. Four published epidemiology studies evaluated the outcomes of a total of 744 women exposed to oral ivermectin in various stages of pregnancy. In the largest study, 397 women in the second trimester of pregnancy were treated open-label with single doses of ivermectin or ivermectin plus albendazole; there was no observed difference in pregnancy outcomes between treated and untreated populations. However, these studies cannot definitely establish or exclude the absence of drug-associated risk during pregnancy, because either the timing of the administration during gestation was not accurately ascertained or the administration only occurred during the second trimester. In animal embyrofetal development studies of oral ivermectin given during organogenesis, adverse developmental outcomes, including cleft palate, exencephaly, wavy ribs, and clubbed forepaws, occurred at or near doses that were maternally toxic. Pre-implantation loss and abortion were also noted.[14][13][15]
Niacinamide
Since niacin is an essential nutrient, one would expect it to be safe when administered during pregnancy at doses meeting the recommended daily allowance (RDA). Niacin is categorized as pregnancy category A under these conditions. However, when used in doses greater than the RDA for dyslipidemia, or when used parenterally for the treatment of pellagra, niacin is categorized as pregnancy category C. Most manufacturers recommend against the use of niacin in dosages greater than the RDA during pregnancy. The potential benefits of high-dose niacin therapy should be weighed against risks, since toxicological studies have not been performed.[5]
Oxymetazoline Hydrochloride
Data are limited regarding use of oxymetazoline during pregnancy. No adequate and well-controlled trials have been conducted, and it is unknown if the drug causes fetal harm or adverse pregnancy outcomes. Data from one literature article found a potential association between second trimester exposure to oxymetazoline nasal spray and renal collecting system anomalies. In another case, fetal distress was reported in a 41-week pregnant patient following repeated use of oxymetazoline nasal spray at a dose 5-times the recommended dose. The fetal distress resolved hours later, and prior to delivery of the healthy infant. Exposure to oxymetazoline topical cream has also been reported in two pregnant females. One pregnancy resulted in delivery of a healthy child. The other pregnancy ended in spontaneous abortion, which was not considered related to drug exposure.[10]
Ivermectin
After oral administration, ivermectin is excreted in human breastmilk in low concentrations. There is insufficient evidence to determine its effects on the breastfed infant or milk production.[13][14]It is estimated that an exclusively breast-fed infant would receive less than 1% of the maternal weight adjusted maternal dose.[16] According to the manufacturer, treatment with oral ivermectin in mothers who are breast-feeding should only be undertaken when the risk of delayed treatment to the mother outweighs the possible risk to the newborn.[13]Previous American Academy of Pediatrics (AAP) recommendations considered oral ivermectin to be usually compatible with breastfeeding.[17] The amount of ivermectin present in human milk after topical application has not been studied; however, systemic exposure from topical ivermectin use is much lower than from oral use. According to the manufacturer, discontinue nursing or discontinue the topical cream, taking into account the importance of the drug to the mother. Consider the developmental and health benefits of breastfeeding along with the mother’s clinical need for the topical lotion and any potential adverse effects on the breast-fed infant from the topical lotion or the underlying maternal condition. Women who are breastfeeding while using topical ivermectin should avoid accidental transfer of ivermectin to the breast area where it might be directly ingested while nursing.[14][15]
Niacinamide
According to a manufacturer of niacin (Niaspan), although no studies have been conducted in nursing mothers, excretion into human milk is expected. The manufacturer recommends the discontinuation of nursing or the drug due to serious adverse reactions that may occur in nursing infants from lipid-altering doses of nicotinic acid.[5] Niacin, in the form of niacinamide, is excreted in breastmilk in proportion to maternal intake. Niacin supplementation is only needed in those lactating women who do not have adequate dietary intake. The Recommended Daily Allowance (RDA) of the National Academy of Science for niacin during lactation is 20 mg.[20] There are no safety data regarding the use of nicotinic acid in doses above the RDA during breastfeeding. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breastfeeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA.
Oxymetazoline Hydrochloride
It is not known whether oxymetazoline is distributed into breastmilk, or if the drug affects breast milk production. According to the manufacturer, caution should be exercised when administering it to women who are breastfeeding their infants. Consider the benefits of breastfeeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breastfeeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA.[10]
Store this medication in its original container at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
- Chouela E, Abeldano A, et el. Arch Dematol 1999;135:651-5.
- del Giudice P, Chosidow O, Caumes E. Ivermectin in dermatology. J Drugs Dermatol 2003;2:13-21.
- Richard-Lenoble D, Chandenier J, and Gaxotte P. Ivermectin and filariasis. Fundam Clin Pharmacology 2003;17:199-203.
- Ottesen EA, Campbell WC. Ivermectin in human medicine. J Antimicrobial Chemotherapy 1994;34:195-203.
- Niaspan (niacin extended-release) tablet package insert. North Chicago, IL: Abbott Laboratories; 2015 Apr.
- HPS2-THRIVE Collaborative Group. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med 2014;371:203-12.
- Taylor AJ, Villines TC, Stanck EJ, et al. Extended-release niacin or ezetimibe and carotid intima-media thickness. N Engl J Med 2009. Epub ahead of print, doi:10.1056/NEJMoa907569.
- Lee JMS, Robson MD, Yu LM, et al. Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: A randomized, placebo-controlled, magnetic resonance imaging study. J Am Coll Cardiol 2009;54:1787—94.
- McKenney JM, et al. A comparison of the efficacy and toxic effects of sustained- vs immediate-release niacin in hypercholesterolemic patients. JAMA 1994;271:672-7.
- Rhofade (oxymetazoline hydrochloride cream) package insert. Irvine, CA: Allergan; 2017 Jan.
- Afrin No Drip Extra Moisturizing (oxymetazoline hydrochloride spray, metered) package insert. Whippany, NJ: Bayer Healthcare LLC; 2016 Aug.
- Visine LR (oxymetazoline hydrochloride 0.025% solution) package insert. Fort Washington, PA: Johnson and Johnson Healthcare Products, Inc.; 2010 Apr.
- Stromectol (ivermectin) package insert. Whitehouse Station, NJ: Merck and Co., Inc.; 2018 Feb.
- Sklice (ivermectin lotion) package insert. Atlanta, GA: Arbor Pharmaceuticals; 2017 Jun.
- Soolantra (ivermectin) package insert. Fort Worth, TX: Galderma Laboratories; 2018 Apr.
- National Institutes of Health (NIH). Ivermectin monograph. LactMed: Drug and Lactation Database. Available at http://toxnet.nlm.nih.gov/cgi-bin/sis/search/f?./temp/~tx6AqM:1. Accessed February 9, 2012.
- American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108(3):776-789.
- Colletti RB, Neufeld EJ, Roff NK, et al. Niacin treatment of hypercholesterolemia in children. Pediatrics 1993;92:78-82.
- Expert Panel: National Cholesterol Education Program. Report of the expert panel on blood cholesterol levels in children and adolescents. Pediatrics 1992;89(suppl 2):525-84.
- Niacinamide. In: Drugs in Pregnancy and Lactation. A Reference Guide to Fetal and Neonatal Risk. Briggs GG, Freeman RK, Yaffe SJ, (eds.) 7th ed., Philadelphia PA: Lippincott Williams and Wilkins; 2005:1140-1
- Health Care Financing Administration. Interpretive Guidelines for Long-term Care Facilities. Title 42 CFR 483.25(l) F329: Unnecessary Drugs. Revised 2015.
- Homeida MM, Bagi IA, Ghalib HW, et al. Prolongation of prothrombin time with ivermectin. Lancet 1988;1:1346-7..
- Whitworth JA, Hay CR, McNicholas AM, et al. Coagulation abnormalities and ivermectin. Ann Trop Med Parasitol 1992;86:301-5.
- Richards FO, McNeely MB, Bryan RT, et al. Ivermectin and prothrombin time. Lancet 1989;1:1139.
- Pacque MC, Munoz B, White AT, et al. Ivermectin and prothrombin time. Lancet 1989;1:1140.
- Niacor (Niacin tablets) package insert. Minneapolis, MN: Upsher-Smith Laboratories, Inc.; 2000 Feb.
- FDA Drug Safety Communication. Over-The-Counter Eye Drops and Nasal Sprays- Serious Adverse Events from Accidental Ingestion by Children. Retrieved Oct. 25, 2012. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm325729.htm?source=govdeliver
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
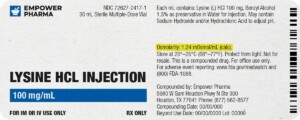
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.


 Acne Keto Cream
Acne Keto Cream Melasma NT Cream
Melasma NT Cream Hair Restore Lite Scalp Solution
Hair Restore Lite Scalp Solution Anti-Aging Vita Gel
Anti-Aging Vita Gel Tretinoin TAAN Cream
Tretinoin TAAN Cream Biotin / Minoxidil / Spironolactone Capsules
Biotin / Minoxidil / Spironolactone Capsules NAD+ Cream
NAD+ Cream Anti-Aging Siro Gel
Anti-Aging Siro Gel Dermatitis TN Cream
Dermatitis TN Cream Scar PT Gel
Scar PT Gel