Melatonin Capsules
This product is available solely through our 503A Compounding Pharmacy, ensuring personalized care and precision in every order. Please note that a valid prescription is required for purchase. If you do not have an account, please contact us.
Product Overview
† commercial product
Melatonin or 5-methoxy-N-acetyltryptamine is a neurohormone used to regulate sleep-wake cycles in patients with sleep disorders. Endogenous melatonin is secreted by the pineal gland in all animals exhibiting circadian or circannual rhythms. Melatonin plays a proven role in maintaining sleep-wake rhythms, and supplementation may help to regulate sleep disturbances that occur with insomnia, jet lag, rotating shift-work, depression, chronic kidney disease, critical care unit stays, and various neurological disabilities. Clinical study of melatonin continues to elucidate the role of melatonin in a variety of neurologic, hormonal, gastrointestinal, and neoplastic disorders The effects of melatonin as a hormone were first noted in 1917, when dark-skinned tadpoles fed a pineal gland extract were noted to develop lighter skin. Melatonin was isolated from the pineal gland in 1958. Commercial melatonin products are primarily synthesized from 5-methoxyindole; rarely, commercial products are derived from animal (bovine) pineal glands. Use of animal based melatonin products is not recommended due to the potential risk of contamination from animal-based infectious prions and viruses, which may cause serious illness. Oral melatonin is included in the Natural Health Products ingredients/monograph database for Health Canada.[1] In Europe, melatonin is available by prescription only under the brand name Circadin, which is marketed as monotherapy for the short-term treatment of primary insomnia characterised by poor quality of sleep in patients who are aged 55 or over.[2] The American Sleep Disorder Association considers melatonin an experimental drug and does not recommend its use without medical supervision. Melatonin has been classified as an orphan drug by the U.S. Food and Drug Administration (FDA) since 1993 for circadian rhythm sleep disorders in blind patients who have no light perception, a condition often known as non-24-hour sleep-wake disorder (non-24), a condition that occurs when the blind patient cannot synchronize their circadian rhythms to a light-dark cycle. In 2013, an additional orphan drug designation was granted by the FDA for the use of melatonin for the treatment of neonatal hypoxic ischemic encephalopathy. Melatonin is also available over the counter in the U.S., and products are marketed under the Dietary Supplement and Health Education Act of 1994 (DSHEA).
NOTE: In the US, nutraceuticals are marketed under the Dietary Supplement and Health Education Act of 1994 (DSHEA). Consequently, scientific data supporting claimed benefit(s) are not always available for nutraceuticals as they are for traditional pharmaceuticals since nutraceuticals are not regulated as drugs. Consumers should also note that rigid quality control standards are not required for nutraceuticals and substantial variability can occur in both the potency and the purity of these products.
Melatonin is an endogenous hormone secreted by the pineal gland. The suprachiasmatic nuclei of the hypothalamus controls the numerous physiologic and endocrine circadian rhythms of the body, including that of rest and activity. The circadian clock is set via a process called entrainment, which is a response of the suprachiasmatic nuclei to photic input. Synthesis and secretion of endogenous melatonin is controlled by enzymes secreted by the hypothalamus which are activated by darkness and depressed by environmental light. Exactly how melatonin induces sleep is not clear, but it is probably not through a direct hypnotic effect. In patients with jet lag or circadian rhythm disorders, endogenous melatonin secretion does not correspond to the social or solar sleep-wake cycles imposed by their surroundings, and they experience sleep disruption. Administration of exogenous melatonin appears to re-set the body to the environmental clock and allow patients to normalize physiologic and behavioral sleep patterns. Exogenous melatonin maximally advances delayed rhythms when administered before endogenous melatonin levels begin to increase in the evening hours. In addition to circadian phase-shifting effects, melatonin has been shown to decrease nocturnal core body temperature, which helps to facilitate sleep. To date, pharmacological tolerance to melatonin has not been described.
Melatonin is involved in other physiologic processes besides the sleep-wake cycle. Secretion of melatonin from the pineal gland is highest during the pediatric years and tends to decrease with age. This age-related secretion performs important endocrine functions. It is thought that higher pre-pubertal melatonin levels are responsible for keeping the hypothalamic-pituitary-gonadal axis in quiescence, and that decreasing melatonin levels with age play a role in the onset of adolescence and sexual maturation. Melatonin receptors have been found in all male and female sexually responsive tissues, indicating that melatonin has a significant role in normal reproductive capacity. Exogenous melatonin can suppress the release of gonadotropin releasing hormone and lutenizing hormone, leading to anovulation and changes in steroid responsive tissues, especially in higher doses. Contraceptive activity has been noted when women are given melatonin in combination with norethindrone.
Melatonin also exhibits immunostimulatory and antioxidant actions. In neurodegenerative disease models, melatonin appears to neutralize oxidizing free radicals, specifically by preventing the reduction of antioxidant enzyme activity, and reducing beta-amyloid mediated lipid peroxidation of cell membranes. These actions appear to decrease apoptosis of neuronal cells. Further research is needed to determine if melatonin may preserve function in neurologic diseases where free radicals have been implicated as partially causative of the conditions. In epilepsy, the rise and fall of endogenous melatonin levels may influence seizure activity. Melatonin may play a role in certain cancers, and in some cases, may have antiproliferative effects on some tumors. The actions and role of melatonin in other body processes, such as regulation of the gastrointestinal system, continues to be investigated. Melatonin may also stimulate the activity of natural killer (NK) cells, lymphocytes, and various cytokines. Further study in well-controlled trials should answer further questions regarding melatonin’s neurologic, immunologic, and oncostatic activities.
If melatonin is going to be used, a synthetic-source product is recommended. Consumers of melatonin should be informed that rigid quality control standards, as with other dietary supplements, are not required for melatonin and substantial variability can occur in both the potency and the purity of these products. Impurities have been found in many dietary supplement products. including melatonin.[3] Impurities may cause allergic reactions or side effects. While melatonin supplements and pharmaceuticals are now almost exclusively produced synthetically, there may be available melatonin supplements derived from the pineal glands of beef cattle, and these should be avoided by those with bovine protein hypersensitivity. The use of animal-source melatonin products is also not recommended due to a potential risk of exposure to infection (e.g., bovine spongiform encephalopathy, also known as “mad cow disease”) or other contamination.[4][5]
Patients who develop angioedema, hypersensitivity or other serious allergic-type events due to melatonin should not be rechallenged with the dietary supplement.[1][2] Patients with asthma should seek health care professional advice prior to melatonin use, as melatonin may play a role in the expression of asthma symptoms.[1]
Melatonin may cause drowsiness. Driving or operating machinery, or performing other tasks that require mental alertness should be avoided after ingestion of melatonin; patients should confine their activities to those necessary to prepare for bed. Sedation occurring after melatonin use during waking hours may indicate excessive dosage. Complex behaviors such as “sleep-driving” (i.e., driving while not fully awake after ingestion of a hypnotic) and other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex), with amnesia for the event, have been reported in association with hypnotic use and have been reported in the use of melatonin analogs.[6] The use of alcohol and other CNS depressants may increase the risk of such behaviors. Patients should also be advised to avoid ethanol ingestion in combination with melatonin as additive effects may occur. Discontinuation of melatonin should be considered for a patient who reports any complex sleep behavior.
Exogenous melatonin should be used with caution in patients with hepatic disease and should be avoided in patients with severe hepatic impairment. Published data demonstrates markedly elevated endogenous melatonin levels during daytime hours due to decreased clearance in patients with hepatic impairment.[2] Patients with hepatic disease should consult their health care provider prior to the use of melatonin.
Melatonin acts on the central nervous system and has sedative effects. Melatonin should be used with caution when patients are being treated for a psychiatric condition or neurological disease, such as a seizure disorder, by a health care professional, particularly if they are on prescription medication for such problems; seizures have been reported as a potential adverse effect of melatonin use.[1][7] Melatonin is not recommended for people who are on prescribed neurologic, psychotropic, or hypnotic medications without the supervision of a qualified health care professional. The failure of insomnia to remit after 7 to 10 days of self-treatment or within 4 weeks of prescription melatonin use may indicate the presence of a primary psychiatric and/or medical illness that should be evaluated. Exacerbation of insomnia and emergence of cognitive and behavioral abnormalities have been seen with melatonin analogs and other hypnotics in clinical use. In primarily depressed patients, worsening of depression (including suicidal ideation and completed suicides) have been reported in association with the use of various hypnotics. As with other melatonin analogs, the emergence of any new changes in mood, cognition, or behavior in a patient taking melatonin requires further evaluation of the patient.[6]
Patients who are undergoing treatment for certain conditions should not use melatonin without a health professional’s supervision due to the potential role of melatonin in hormonal, cellular, and immunomodulatory functions. For example, melatonin appears to influence insulin, glucose, lipid metabolism and antioxidant capacity and thus melatonin supplements may influence glycemic control in patients with diabetes mellitus. Patients with diabetes should monitor their blood sugar. Patients with various other types of endocrine disease should get approval of their health care provider prior to use. There is also evidence that melatonin influences the regulation of certain types of cancer, and until these effects are more fully understood, patients with breast cancer or other neoplastic disease should only use melatonin with the approval of their cancer specialist. Melatonin is not recommended for use in patients with autoimmune disease or a history of organ transplant due to lack of clinical data and a lack of interaction data with drugs used to treat these conditions.[1][2]
As a hormone, melatonin modulates steroid hormone actions, including those in reproductive and mammary tissues. Melatonin and melatonin analogs have been associated with an effect on reproductive hormones in adults (e.g., decreased testosterone levels and increased prolactin levels). It is not known how chronic or intermittent chronic use of melatonin affects reproductive risk or development in males or females.[6] Melatonin appears to have important in the regulation of sperm counts, and also has effects related to ovulation in females. Until more is known about its effects on fertility, male and female patients with infertility and those patients who are trying to conceive should avoid melatonin unless their prescriber recommends supplementation.
Melatonin should be considered to be contraindicated in pregnancy at this time.[1] In pregnant women, endogenous melatonin crosses the placenta and enters the fetal circulation, and appears to be responsible for setting circadian rhythm influences in utero. Melatonin receptors in the fetus are widespread in both central and peripheral tissues from the third week of fetal development. The administration of exogenous melatonin could potentially disrupt circadian entrainment and other pineal gland influences.[8] Thus, fetal exposure to exogenous melatonin use in the mother may be of concern. Effects in non-clinical animal studies of melatonin were observed only at exposures considered sufficiently in excess of the maximum human exposure indicating little relevance to clinical use; however, the data are limited.[2] In animal studies, ramelteon, a melatonin analog, produced evidence of developmental toxicity, including teratogenic effects, in rats at doses much greater than the recommended human dose.[6] The potential effects of melatonin on the duration of labor and/or obstetric delivery, for either the mother or the fetus, have not been studied. Melatonin has no established use in labor and delivery.
Melatonin should generally be avoided in women who are breast-feeding their infants.[1][2] Reports describing the use of melatonin dietary supplements in women who are breast-feeding are lacking; however, it is likely to be excreted in human milk. Endogenous melatonin passes into human milk and concentrations have been measured in the breast-milk of lactating women; the results coincided with the women’s daily circadian rhythm of melatonin with undetectable levels during the day and high levels at night.[9]
Safety and efficacy of melatonin have not been established in pediatric patients under 18 years of age.[2] Due to a lack of scientific data and an unknown potential for side effects, melatonin should not be used in infants or very young children. Further study is needed to determine if melatonin may be used safely in pre-pubescent and pubescent pediatric patients. Several small, randomized controlled trials suggest the efficacy and relative safety of short-term supplemental melatonin in treating insomnia in children who have autism spectrum disorders (ASD) and other neurologic disorders; however, experts agree larger studies are needed. [10][11] Melatonin and melatonin analogs have been associated with an effect on reproductive hormones in adults (e.g., decreased testosterone levels and increased prolactin levels). It is not known what effect chronic or intermittent chronic use of melatonin would have on the reproductive and gonadal function of pre-pubescent or pubescent pediatric patients.[6] Education regarding proper sleep hygiene and establishing developmentally appropriate and consistent bedtime schedules are first-line interventions for any child. Caregivers are encouraged to seek the advice of the health care provider prior to the use of melatonin in children.
Most central nervous system (CNS) adverse effects of melatonin appear to be infrequent and mild in most patients with a few days of use. Much less is known regarding side effects occurring during the long term melatonin administration. Most clinical trials have involved <= 6 months of daily melatonin use. The most commonly reported adverse reactions are headache and somnolence. Prolonged sedation and drowsiness during waking hours have been noted; patients experiencing excessive drowsiness during waking hours following melatonin use at bedtime may need to consume a lower bedtime dosage. One study reported that subjective drowsiness from melatonin may affect attention and concentration while driving; patients should determine how melatonin affects them before participating in activities requiring alertness. Other CNS and psychiatric adverse reactions include dizziness, abnormal dreams, unspecified sleep disturbances, nightmares, and seizures in the published literature.[7] In primarily depressed patients, worsening of depression (including suicidal ideation) have been reported. Hallucinations, as well as behavioral changes such as bizarre behavior, anxiety, agitation, and mania have been reported with the use of melatonin analogs.[6] Neuro-psychiatric symptoms may occur unpredictably. Complex sleep-related behaviors such as "sleep-driving" (i.e., driving while not fully awake after ingestion of a hypnotic) and other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex), with amnesia for the event, have been reported in association with hypnotic use, including melatonin analogs.[6] The use of alcohol and other hypnotics should be avoided when possible since these may increase the risk of such symptoms. Somnambulism (sleep walking) has been reported when melatonin was used in conjunction with zolpidem. As with other melatonin analogs, the emergence of any new changes in mood, cognition, or behavior requires further evaluation of the patient. Discontinuation of melatonin should be considered for patients who report any complex sleep behavior, worsening depression, or any other unusual changes in moods or behaviors. During excessive melatonin dosage (e.g., 24 to 30 mg of ingestion), impaired cognition, lethargy, disorientation, short-term amnesia, acute psychosis and confusion have been reported.[12][13] In these cases, the temporal association of melatonin ingestion to the clinical course of the patients supported melatonin as the causative agent. Gastrointestinal (GI) adverse effects of melatonin appear to be infrequent with a few days of use. Much less is known regarding the long term administration of this hormone. Most clinical trials have involved <= 6 months of daily melatonin administration. Infrequent or rare GI adverse reactions reported in the published literature include abdominal pain, dyspepsia, pyrosis (heartburn), nausea, vomiting, constipation, flatulence, and difficulty swallowing.[7] Melatonin may rarely cause allergic or dermatologic reactions. Rash (unspecified), including fixed drug eruptions and exanthema, with or without pruritus, have been reported after melatonin administration. Other reported dermatologic effects include hyperhidrosis (increased sweating) and hot flashes. Rarely, angioedema and anaphylactoid reactions have been reported with the melatonin analog, ramelteon; however, no reports of such reactions to melatonin are found in the published literature.[6] A report of "difficulty swallowing and breathing" was reported in one clinical study of melatonin for jet lag; this might have represented an allergic response. Patients experiencing a serious allergic reaction to melatonin should discontinue the agent and not be rechallenged. Cardiovascular (CV) adverse effects of melatonin appear to be infrequent or rare with a few days of use. Much less is known regarding the long term administration of this hormone. Most clinical trials have involved <= 6 months of daily melatonin administration. Infrequent or rare CV reactions reported in the published literature include palpitations and sinus tachycardia. One case report exists in the literature describing a temporal association of melatonin use for insomnia with the development of autoimmune hepatitis confirmed by liver biopsy. Discontinuation of the melatonin and the administration of corticosteroid therapy resulted in symptomatic and clinical improvements.[14] A case of autoimmune hepatitis has been reported in the literature due to ramelteon, a melatonin agonist.[15] Adverse events reported with melatonin appear to be infrequent or rare with a few days of use. Much less is known regarding the long term administration of this hormone. Most clinical trials have involved <= 6 months of daily melatonin administration. Infrequent or rare general adverse reactions reported in the published literature include naso-pharyngitis, arthralgia, and swelling of the arms/legs (fluid retention) following air travel.
Melatonin should be considered to be contraindicated in pregnancy at this time.[1] In pregnant women, endogenous melatonin crosses the placenta and enters the fetal circulation, and appears to be responsible for setting circadian rhythm influences in utero. Melatonin receptors in the fetus are widespread in both central and peripheral tissues from the third week of fetal development. The administration of exogenous melatonin could potentially disrupt circadian entrainment and other pineal gland influences.[8] Thus, fetal exposure to exogenous melatonin use in the mother may be of concern. Effects in non-clinical animal studies of melatonin were observed only at exposures considered sufficiently in excess of the maximum human exposure indicating little relevance to clinical use; however, the data are limited.[2] In animal studies, ramelteon, a melatonin analog, produced evidence of developmental toxicity, including teratogenic effects, in rats at doses much greater than the recommended human dose.[6] The potential effects of melatonin on the duration of labor and/or obstetric delivery, for either the mother or the fetus, have not been studied. Melatonin has no established use in labor and delivery.
Melatonin should generally be avoided in women who are breastfeeding their infants.[1][2] Reports describing the use of melatonin dietary supplements in women who are breastfeeding are lacking; however, it is likely to be excreted in human milk. Endogenous melatonin passes into human milk and concentrations have been measured in the breastmilk of lactating women; the results coincided with the women’s daily circadian rhythm of melatonin with undetectable levels during the day and high levels at night.[9]
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond use date. Do not flush unused medications or pour down a sink or drain.
- Health Canada Drugs and Health Products and Natural Health Products Ingredients Database. Melatonin Monograph. First published 2012. Modified May 13, 2013. Web. Accessed August 4, 2015. Available at: webprod.hc-sc.gc.ca/nhpid-bdipsn.
- Circadin (oral melatonin) European Medicines Agency official product label. Dublin 2, Republic of Ireland; Flynn Pharma Ltd: 2015 July.
- Williamson BL, Tomlinson AJ, Mishra PK, et al: Structural characterization of contaminants found in commercial preparations of melatonin:similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem
- Naylor S, Gleich GJ. Over-the-counter melatonin products and contamination. Am Fam Physician. 1999;59:284, 287-8.
- Norton SA. Raw animal tissues and dietary supplements. N Engl J Med 2000;343:304–305.
- Rozerem (ramelteon) package insert. Lincolnshire, IL: Takeda Pharmaceuticals; 2010 Nov.
- Waldron DL, Bramble D, Gringras P: Melatonin: Prescribing practices and adverse events. Arch Dis Child 2005;90(11):1206-1207.
- Davis FC. Melatonin: role in development. J Biol Rhythms 1997;12:498-508.
- Illnerova H, Buresova M, Presl J. Melatonin rhythm in human milk. J Clin Endocrinol Metab 1993;77:838—41.
- Chase JE, Gidal BE. Melatonin: therapeutic use in sleep disorders. Ann Pharmacother 1997;31:1218-26.
- McArthur AJ, Budden SS. Sleep dysfunction in Rett Syndrome: a trial of exogenous melatonin treatment. Dev Med Child Neurol 1998;40:186-92.
- Holliman BJ, Chyka PA. Problems in assessment of acute melatonin overdose. South Med J 1997;90:451-3.
- Force RW, Hansen L, Bedell M. Psychotic episode after melatonin. Ann Pharmacother 1997;31:1408.
- Hong YG, Riegler JL. Is melatonin associated with the development of autoimmune hepatitis? J Clin Gastroenterol 1997;25:376-8.
- Fourman LT, Robert Meyer B. Autoimmune hepatitis in association with ramelteon. J Clin Gastroenterol. 2013 Apr 29. [Epub ahead of print]
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
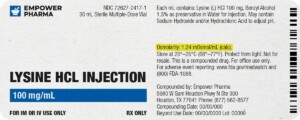
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.


 NAD+ Nasal Spray
NAD+ Nasal Spray Coenzyme Q10 (Ubidecarenone) Injection
Coenzyme Q10 (Ubidecarenone) Injection Propranolol Tablets
Propranolol Tablets Vitamin B-Complex Injection
Vitamin B-Complex Injection Niacin SR Tablets
Niacin SR Tablets DMSA (Succimer) Capsules
DMSA (Succimer) Capsules Ezetimibe Tablets
Ezetimibe Tablets DHEA / Pregnenolone Capsules
DHEA / Pregnenolone Capsules Methylcobalamin Injection (Vitamin B12)
Methylcobalamin Injection (Vitamin B12) BCAA Injection
BCAA Injection