Who We AreMaking our mark on the healthcare landscape
At Empower, we’re on a mission to innovate the healthcare industry and propel it into the future.

Purpose, Vision, and Mission
Our Purpose
To be a catalyst for positive change in the healthcare landscape and revolutionize the accessibility of medicine.
Our Vision
To expand access to quality, affordable medication.
Our Mission
To produce innovative medications to help people live healthier, happier lives.
OUR VALUES
Our people define who we are as a company, and we believe that understanding and addressing the needs of our team, clients, and community is fundamental to fostering a culture of support and growth.

Quality stands at the core of our mission, reflecting our commitment to excellence in every medication we produce. We uphold the highest standards of safety and efficacy, ensuring the communities we serve receive our best.

We are here to serve others. Every interaction with our patients, providers, employees and other stakeholders comes from a place of service.

By continuously exploring new methodologies and embracing technology, we ensure that every solution we offer is at the forefront of pharmaceutical care.
Our Credo
We believe our foremost responsibility is to the patients, providers, and caregivers who rely on our medications and services. Every product we create, every action we take, must be rooted in a commitment to quality, affordability, and accessibility. We understand that behind every order is a person in need, and with that knowledge, we strive for excellence in all that we do.
Our PeopleMeet our leaders
We pride ourselves on the combined expertise of our leaders.
Shaun Noorian
Founder, CEO & ChairmanShaun Noorian is leading a national movement to restore trust, access, and innovation in healthcare. Under his leadership, Empower has become the largest and most advanced 503A compounding pharmacy and 503B outsourcing facility in the country, serving patients and providers across all 50 states.
At the core of Shaun’s work is a belief that people deserve personalized medicine, transparent pricing, and a pharmacy partner that never cuts corners. His team is building the infrastructure and systems to deliver on that promise combining cutting-edge automation, relentless quality, and a patient-first mindset.
Shaun is not just scaling a company. He’s building a new standard for what healthcare can be: affordable, accessible, and anchored in integrity.
Bob Irwin
PresidentBob Irwin believes people are the heart of Empower’s mission. He fosters an environment where individuals thrive, aligning with a shared purpose to deliver lasting value to themselves, their families, and their communities.
Empower’s vision to provide access to quality, affordable medication for 300 million people drives Bob and his team as they expand their impact on the pharmaceutical industry. His leadership is rooted in authenticity, strategic execution, and cultivating a strong, inclusive culture.
Outside of work, Bob enjoys Ohio State football, golfing, time on the water, traveling, and reflecting on leadership.
Edgar Gonzalez
General CounselEdgar Gonzalez brings a strong legal background with extensive experience in national security law, cybersecurity, data privacy, and mergers & acquisitions. He is responsible for overseeing all legal affairs at Empower, ensuring compliance with federal regulations, and managing corporate governance, intellectual property, and litigation matters.
Before joining Empower, Edgar served as a JAG Attorney with the U.S. Coast Guard for over 10 years, where he advised on military justice, maritime law, and government affairs. He also held the position of Senior Associate at Patterson + Sheridan, focusing on intellectual property litigation and patent prosecution. Edgar’s legal career includes roles with Abraham, Watkins, Nichols, Agosto, Aziz & Stogner and the United States Attorneys’ Offices, where he handled complex criminal and civil cases.
Edgar’s broad legal experience, combined with his dedication to empowering organizations through strategic legal counsel, supports Empower’s mission of delivering quality, affordable medications nationwide.
Jonathan Abrarpour
Chief Operating OfficerJonathan Abrarpour oversees the daily operations of the nation’s largest 503A compounding pharmacy and 503B outsourcing facility. Empower’s state-of-the-art infrastructure and strict adherence to FDA cGMP standards ensure the delivery of quality, personalized medications nationwide.
Jonathan collaborates with department leaders to optimize processes, execute strategic initiatives, and ensure operational excellence. His leadership has been instrumental in enhancing efficiency, fostering continuous improvement, and supporting Empower’s rapid growth.
A Texas Tech University graduate with a B.S. in Mechanical Engineering, Jonathan began his career at ConocoPhillips before joining Empower in 2015. He later advanced as Chief Production Officer, further solidifying Empower’s leadership in the industry.
Jonathan is passionate about mentorship and professional development, driving innovation and ensuring Empower remains at the forefront of healthcare manufacturing.
Valerie Capers Workman
Chief Human Resources OfficerValerie Capers Workman leads the company’s people strategy to support its mission of expanding access to affordable, quality medications. She brings expertise in workforce transformation, AI integration, and leadership development, helping Empower scale responsibly while creating opportunity for its growing team.
Before joining Empower, Valerie held executive roles at Tesla and Handshake, where she led large-scale talent, compliance, and engagement initiatives. A licensed attorney in New York, Texas, and Washington, D.C., she also serves on the Board of Trustees for Huston-Tillotson University and the S.I Newhouse Advisory Board for Syracuse University.
A best-selling author and global speaker, Valerie is passionate about building inclusive, AI-enabled workplaces that shape the future of work.
Dalbir Singh
Chief Talent OfficerDalbir Singh leads the company’s talent strategy to support its mission of expanding access to affordable, quality medications. He focuses on building strong leadership pipelines, building engaged teams, and connecting talent development to business success.
With over two decades of experience spanning North America, Europe, and Asia, Dalbir has guided organizations through large-scale transformation and global expansion. He has held leadership roles at Zapata AI, Expedia, GE, Flipkart, Microsoft, CSC, and HCL, where he built high-performing teams and advanced organizational capabilities.
A certified leadership coach and advisor, Dalbir is passionate about developing talent and shaping environments where people and businesses thrive. His approach combines strategic vision with hands-on execution, helping Empower scale responsibly while investing in its people.
Jasen Bruce
Chief Strategic Growth OfficerJasen Bruce leads Empower’s strategic growth and partnership initiatives, expanding national access to quality, affordable medication. With more than two decades of experience spanning Integrative Health, Pharmacy Operations, and Provider Services, Jasen has been instrumental in shaping how telemedicine practices, pharmacies, and physicians collaborate to deliver personalized care.
Before rejoining Empower, Jasen founded and led multiple organizations at the intersection of medicine and business, including Defy Medical, which helped pioneer integrative treatment models and nationwide provider support programs. His background combines clinical operations, sales leadership, and product development, giving him a unique perspective on how innovation translates into real-world patient outcomes.
A former U.S. Marine, Jasen brings a mission-driven mindset to every role defined by discipline, trust, and service. Under his leadership, Empower’s growth strategy centers on strengthening provider relationships, elevating clinical education, and redefining what integrity and transparency look like in pharmaceutical care.
Thomas George
Chief Sales OfficerThomas George leads the company’s commercial transformation, redefining how healthcare organizations scale through disciplined strategy, advanced technology, and a patient-first mindset. His leadership drives Empower’s mission to expand access to quality, affordable compounded medications nationwide.
Thomas and his team are building the revenue engine that powers Empower’s growth, integrating AI-driven insights, operational excellence, and authentic leadership to deliver meaningful impact for providers and patients alike.
He holds a B.A. from Rutgers University, an M.S. from Stevens Institute of Technology, and an MBA from Northwestern University’s Kellogg School of Management. With a foundation that blends technical depth and strategic vision, Thomas believes sustainable growth happens where innovation, data, and purpose intersect creating environments where teams thrive and healthcare becomes more personal.
Jaspreet Singh
Chief Customer OfficerJaspreet Singh leads Empower’s Customer Success strategy, driving a company-wide commitment to transparent, personalized support and a “Customer First” mindset. With nearly three decades of global experience across Sales, Customer Success, Consulting, and Support, he ensures Empower delivers measurable value and builds long-term partnerships with providers nationwide.
Before joining Empower, Jaspreet served as Vice President of Customer Technical Success at Autodesk, where he led technical adoption, services, and support during a period of rapid growth. He previously spent more than 17 years at Microsoft, holding leadership roles across Customer Success, global support, and enterprise sales strategy, and managing teams across multiple continents.
Jaspreet is passionate about people development, organizational culture, and leadership coaching. He is a certified ICF coach and has guided numerous initiatives focused on diversity, inclusion, and talent development.
He holds an engineering degree with honors from the National Institute of Technology in Jalandhar and completed an executive management program at the Indian Institute of Management, Bengaluru. Jaspreet and his family enjoy traveling, music, and exploring cuisines from around the world.
By expanding access to quality, affordable medication, we are opening doors for providers, patients, and other pharmacies like never before.
Our GrowthA history of growth and innovation

Empower Pharmacy is Born
Shaun Noorian, our founder & CEO starts Empower Pharmacy with a vision to provide access to quality, affordable medication to patients like himself.

New Pharmacy Constructed
Empower expands from a 150-square-foot space to a 1,500-square-foot facility, featuring our first cleanroom. This advancement allows us to broaden our formulary to include both nonsterile and sterile compounded preparations, enhancing our ability to serve healthcare providers and improve patient care.

New Standards
With the passage of the Drug Quality and Security Act, which establishes the 503B outsourcing facility category, we take action to lead the industry. We begin construction on our first 503B outsourcing facility, ensuring patients and providers have access to the highest quality medications with the utmost safety and compliance.

Nationwide Licensure
We secure licensure in all 50 states, ensuring patients nationwide have access to our quality compounded medications. This achievement marks a major step in our mission to expand personalized care and improve health outcomes on a national scale.

FDA Registration
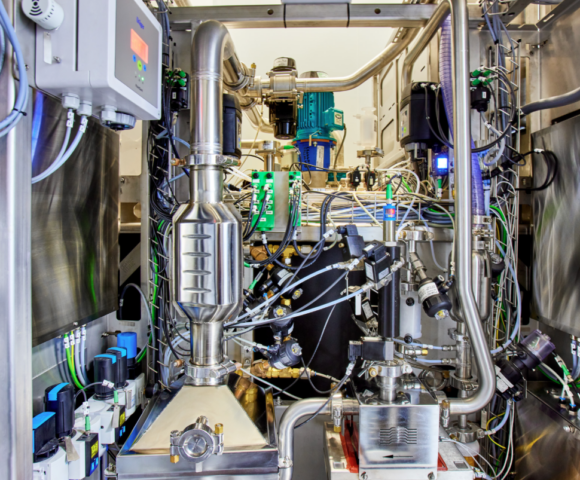
We open our first 503B Outsourcing Facility, built to current Good Manufacturing Practices and designed for seamless scalability through automation. This milestone strengthens patient safety, enhances product quality, and reinforces our commitment to delivering the highest standard of care.

Design and Construction Continue
Empower breaks ground on the largest and most advanced 503A compounding pharmacy in the nation—and the world. This state-of-the-art facility is designed to revolutionize the compounded pharmaceutical supply chain, leveraging cutting-edge automation and innovation to enhance quality, safety, and efficiency. By setting a new global standard in personalized medicine, we are ensuring greater access to life-changing treatments for patients everywhere.

Historic Achievement
Empower becomes the nation’s largest human drug compounding pharmacy, redefining personalized medicine with unmatched scale, quality, and innovation. This milestone strengthens our commitment to providing patients and providers with superior, customized treatments.

New Compounding Pharmacy
We launch the nation’s largest and most advanced compounding pharmacy, leveraging cutting-edge automation to enhance patient safety, ensure unmatched quality, and expand access to personalized medications. This breakthrough allows us to serve millions of patients nationwide with the reliable, life-changing treatments they need for decades to come.

Expanding Access
Empower Pharmacy reaches a major milestone, filling 15,000 custom-compounded prescriptions daily. By delivering personalized medications at this scale, we are transforming patient care, enhancing health outcomes, and redefining the future of pharmacy.

Facility Acquisition
We significantly expand our 503B capabilities with the acquisition of a state-of-the-art, 170,000-square-foot pharmaceutical manufacturing facility in New Jersey. This milestone establishes us as the nation’s largest and most advanced outsourcing facility, increasing our sterile manufacturing capacity more than 20-fold. With this expansion, we are revolutionizing the pharmaceutical industry and ensuring more patients have access to quality, life-changing medications at scale.



