Testosterone Cypionate Injection
Product Overview
† commercial product
Testosterone cypionate is a long-acting esterified form of the endogenous androgen testosterone formulated in grapeseed oil for intramuscular administration; it is compounded in concentrations ranging from 20 mg/mL to 200 mg/mL across 1 mL, 2·5 mL, 5 mL, 10 mL and 30 mL multi-dose vials, allowing prescribers to match dose and vial size precisely to patient requirements[1].
As an individualized preparation produced under sections 503A or 503B of the U.S. Federal Food, Drug, and Cosmetic Act, each batch may be tailored for a single named patient or manufactured in larger lots for office use, yet in both scenarios the formulation must meet pharmaceutical quality standards for sterility, potency and particulate control[2].
Clinically, compounded testosterone cypionate is prescribed for adult males with confirmed hypogonadism who exhibit symptoms such as reduced muscle mass, diminished libido, erectile dysfunction, fatigue or mood disturbance and in whom morning serum testosterone levels on two separate days fall below the young-adult reference range[3].
Because the product is an anabolic-androgenic steroid classified as a Schedule III controlled substance it may only be dispensed pursuant to a valid prescription, must be stored securely and is subject to state and federal monitoring programs aimed at preventing diversion and misuse[4].
The compounded nature of the formulation means inactive components, usually limited to grapeseed oil and possibly a bacteriostatic agent, can be adjusted to address allergies or other patient-specific considerations, thereby offering flexibility beyond what is available with a single commercial brand while still requiring physician oversight and periodic laboratory monitoring to ensure both efficacy and safety[5].
Typical initiation for primary or secondary hypogonadism in adult males is 100 mg to 200 mg injected intramuscularly every two weeks, though some clinicians favour 50 mg weekly to minimise peak-trough fluctuations; serum testosterone is rechecked after two injection intervals and the dose or frequency is adjusted to maintain trough levels in the mid-normal adult range while avoiding supraphysiologic peaks[9].
Deep intramuscular administration into the gluteal muscle using a 22-gauge needle is recommended, and patients who self-inject must be trained in aseptic technique, site rotation and safe sharps disposal to reduce infection and tissue-injury risk[6].
After deep intramuscular injection the lipophilic ester diffuses slowly from the oil depot, undergoes enzymatic cleavage to free testosterone and enters the systemic circulation, where roughly 98 % is reversibly bound to sex-hormone-binding globulin and albumin while the unbound fraction translocates across cell membranes to activate androgen receptors[6] .
Ligand-bound androgen receptor complexes dimerize, migrate to the nucleus and modulate transcription of target genes governing protein synthesis, erythropoiesis, bone mineralization, libido and secondary sexual characteristics; some intracellular testosterone is converted by 5-alpha reductase to the more potent dihydrotestosterone, whereas in adipose tissue a proportion aromatizes to estradiol, supporting skeletal maturation and feedback control of gonadotropins[7] .
Administration therefore restores physiologic androgen levels, suppresses hypothalamic gonadotropin-releasing hormone and pituitary luteinizing hormone, stabilizes nitrogen balance, increases lean body mass and may improve mood and sexual function, yet prolonged suppression of intratesticular testosterone can reduce spermatogenesis, underscoring the need for careful dose titration and fertility counseling when indicated[8].
Testosterone cypionate is contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate because exogenous androgens can stimulate androgen-dependent malignant tissue growth[8].
It must not be administered to patients with hypersensitivity to testosterone, grapeseed oil or any component of the formulation, or to women who are pregnant, could become pregnant or are breastfeeding owing to the risk of virilization and other fetal or neonatal harm[7].
Androgen therapy can potentiate the hypoglycaemic effect of insulin and oral antidiabetic agents, necessitating closer monitoring of fasting glucose and possible dose reductions when testosterone replacement is initiated in diabetic patients[6].
Concomitant use with oral anticoagulants such as warfarin may enhance anticoagulation and alter international normalised ratio values, so prothrombin time should be reviewed more frequently following dose changes of either drug[9].
Co-administration with glucocorticoids or adrenocorticotropic hormone may exacerbate fluid retention and oedema; similarly, potent CYP3A4 inhibitors could raise serum testosterone concentrations, whereas 5-alpha-reductase inhibitors counteract androgenic activity, highlighting the importance of comprehensive medication reconciliation at each visit[10].
Common adverse reactions include transient injection-site discomfort, acne, seborrhoea, increased body hair, mild fluid retention and elevations in haematocrit that may require dose reduction or therapeutic phlebotomy if haematocrit exceeds 54 %[3].
Prolonged therapy can unmask or exacerbate benign prostatic hyperplasia, raise prostate-specific antigen, worsen untreated obstructive sleep apnoea and is associated in some observational studies with a small but controversial increase in cardiovascular events, underlining the necessity for baseline and periodic monitoring of PSA, lipids and cardiovascular risk factors[8].
Exogenous testosterone is teratogenic, capable of inducing virilisation of a female fetus when administered during pregnancy; therefore the drug is absolutely contraindicated in women who are or may become pregnant and exposure during gestation mandates immediate discontinuation and medical evaluation[7].
Because testosterone and its metabolites could be excreted into breast milk and might suppress lactation or adversely affect a nursing infant, therapy is likewise contraindicated during breastfeeding and should not be used in women for routine androgen replacement[4].
Store vials upright at controlled room temperature of 20 °C to 25 °C; protect from light by keeping the vial in its carton and never freeze the oil solution, as crystallisation or vial breakage can occur at sub-zero temperatures[10].
- Bhasin, S., Brito, J. P., et al. (2018). Testosterone therapy in men with hypogonadism: an Endocrine Society clinical practice guideline. *Journal of Clinical Endocrinology & Metabolism*, 103(5), 1715-1744. https://doi.org/10.1210/jc.2018-00229
- Saad, F., Gooren, L. (2017). The role of testosterone therapy in hypogonadal men with obesity and metabolic syndrome. *Journal of Sexual Medicine*, 14(8), 963-971. https://doi.org/10.1016/j.jsxm.2017.05.013
- Morales, A., Johnston, B., Heaton, J. (2015). Intramuscular testosterone: dosing, safety and efficacy. *Canadian Urological Association Journal*, 9(11-12), 400-405.
- Goodman, N., Guay, A., & Dandona, P. (2018). American Association of Clinical Endocrinologists guidelines for management of hypogonadism. *Endocrine Practice*, 24(7), 633-650. https://doi.org/10.4158/GL-2018-030
- Eisenberg, M. L. (2022). Testosterone therapy and male fertility. *Nature Reviews Urology*, 19(9), 505-518. https://doi.org/10.1038/s41585-022-00619-1
- Nieschlag, E., & Vorona, E. (2015). Testosterone and pregnancy: a review. *Reproductive Biology and Endocrinology*, 13(83), 1-11. https://doi.org/10.1186/s12958-015-0084-z
- Kloner, R. A., Carson, C., et al. (2020). Testosterone therapy and cardiovascular outcomes: a comprehensive review. *Current Urology Reports*, 21(5), 33. https://doi.org/10.1007/s11934-020-00985-z
- Sarkar, M., Sengers, B. (2020). Cardiovascular risk associated with testosterone-boosting therapy: a systematic review. *American Journal of Medicine*, 133(4), 389-404.e2. https://doi.org/10.1016/j.amjmed.2019.09.010
- Traish, A. M. (2016). Testosterone therapy in men with testosterone deficiency: Are we beyond the point of no return? *Investigative and Clinical Urology*, 57(6), 384-400. https://doi.org/10.4111/icu.2016.57.6.384
- U.S. Food & Drug Administration. (2021). Testosterone cypionate injection prescribing information.
Because testosterone cypionate is a controlled substance with abuse potential, it should be secured to prevent diversion and any unused or expired product returned to a take-back programme or disposed of in accordance with local pharmaceutical waste guidelines[5].
How long do I need to stay on therapy?
Testosterone deficiency is usually a chronic condition; continuation beyond three to six months depends on symptomatic benefit and laboratory confirmation of necessity, and therapy may be indefinite when tolerated and beneficial[1].
Why is grapeseed oil used as the carrier?
Grapeseed oil has a favourable viscosity for injection, minimal allergenic potential and sufficient solubility for lipophilic esters, making it a common vehicle for compounded testosterone preparations[4].
Does insurance cover compounded testosterone?
Coverage policies vary; some payers reimburse only FDA-approved commercial versions, whereas others cover compounded prescriptions when medically justified and accompanied by documentation of a clinical need that cannot be met by a manufactured product[9].
Can I drink alcohol while on testosterone?
Moderate intake is unlikely to interact directly, but heavy alcohol use may exacerbate hepatic strain and counteract metabolic benefits of therapy, so patients are advised to limit consumption[8].
Are there alternatives if injections are inconvenient?
Transdermal gels, patches and longer-acting subcutaneous implants exist, each with distinct pharmacokinetics and adherence considerations; the choice depends on patient preference, absorption characteristics and cost[5].
Will therapy affect fertility?
Exogenous testosterone suppresses luteinising hormone and intratesticular testosterone, which can decrease sperm production; men wishing to preserve fertility may require concomitant gonadotropin therapy or alternative management strategies[7].
What if I miss an injection?
Administer the dose as soon as remembered unless the next scheduled dose is imminent; never double the dose, and consult your provider for specific guidance if more than one dose has been missed[3].
Can the injections be given subcutaneously?
Some clinicians have reported successful use of small-volume subcutaneous injections, yet the formulation is approved and most widely studied for deep intramuscular delivery, so any off-label route should be discussed carefully with the prescriber[6].
How soon will I feel benefits?
Energy and libido may improve within a few weeks, whereas changes in body composition and bone density may require several months of consistent therapy, reflecting the prolonged half-life of testosterone cypionate and gradual physiologic adaptation[2].
Do I need routine lab work while on therapy?
Yes-baseline and periodic checks of serum testosterone, haematocrit, liver enzymes and prostate-specific antigen allow clinicians to titrate the dose and detect emerging adverse effects early[1].
How long do I need to stay on therapy?
Testosterone deficiency is usually a chronic condition; continuation beyond three to six months depends on symptomatic benefit and laboratory confirmation of necessity, and therapy may be indefinite when tolerated and beneficial[1].
Disclaimer: This compounded medication is prepared under section 503A and 503B of the U.S. Federal Food, Drug, and Cosmetic Act. Safety and efficacy for this formulation have not been evaluated by the FDA. Therapy should be initiated and monitored only by qualified healthcare professionals.
Administration Instructions

Intramuscular Injection Instructions

Subcutaneous Injection Instructions
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.






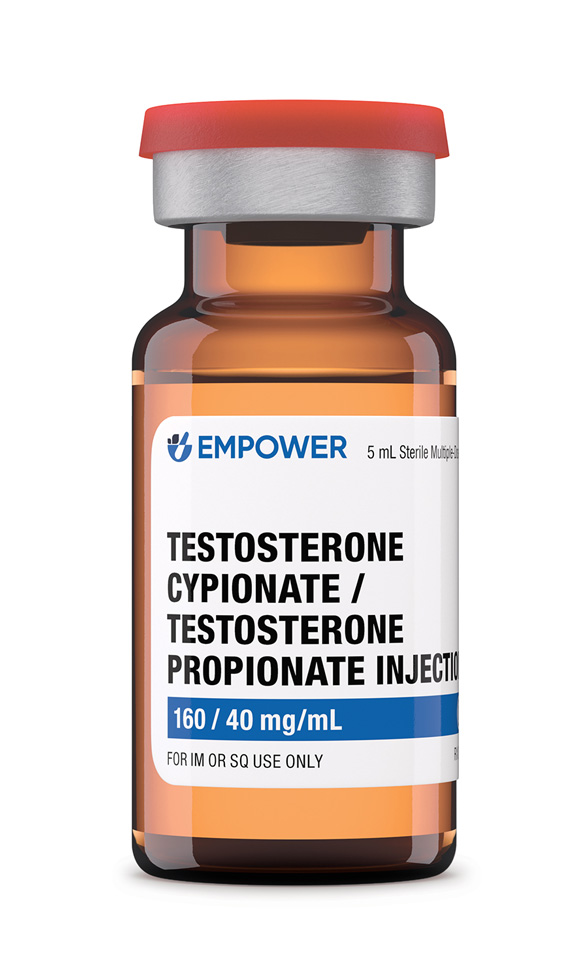 Testosterone Cypionate / Testosterone Propionate Injection
Testosterone Cypionate / Testosterone Propionate Injection Testosterone Cream
Testosterone Cream Anastrozole Capsules
Anastrozole Capsules Enclomiphene Citrate Capsules
Enclomiphene Citrate Capsules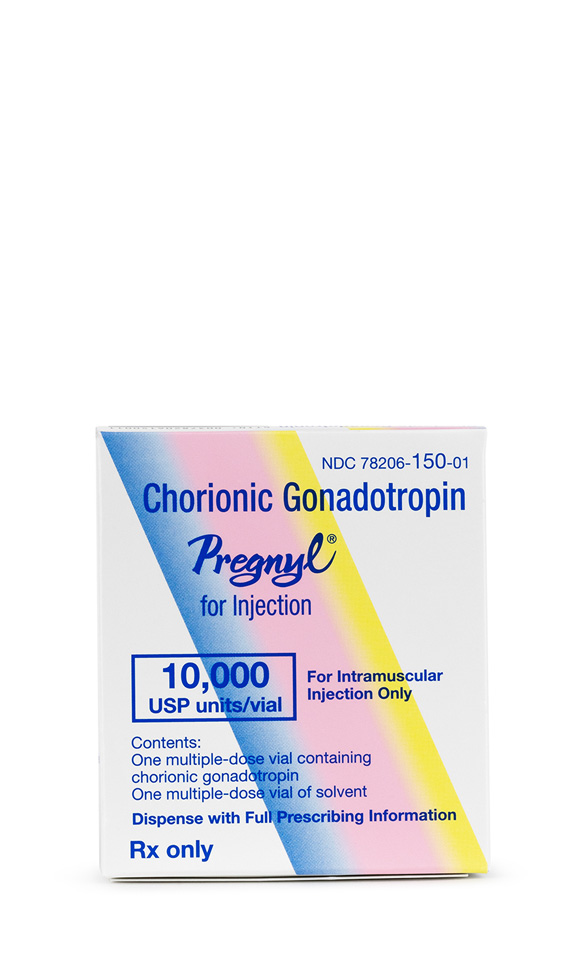 HCG Injection
HCG Injection Sermorelin Acetate Injection
Sermorelin Acetate Injection